Medication Interaction Checker
Check for dangerous interactions
Enter up to two medications to see if they interact. Based on FDA-approved guidelines.
How it works
Based on article information about pharmacokinetics and drug interactions. This tool identifies:
- Drugs that affect metabolism (like CYP450 enzymes)
- Drugs that compete for kidney/liver processing
- Combinations that increase bleeding risk
Every year, millions of people take medications to feel better - but many end up feeling worse. A headache pill gives you nausea. An antibiotic causes a rash. A blood pressure medicine makes you dizzy. It’s not just bad luck. These aren’t random mistakes. They’re predictable outcomes of how drugs interact with your body at a molecular level. Understanding why this happens isn’t just academic - it’s the difference between safe treatment and serious harm.
What Exactly Are Side Effects?
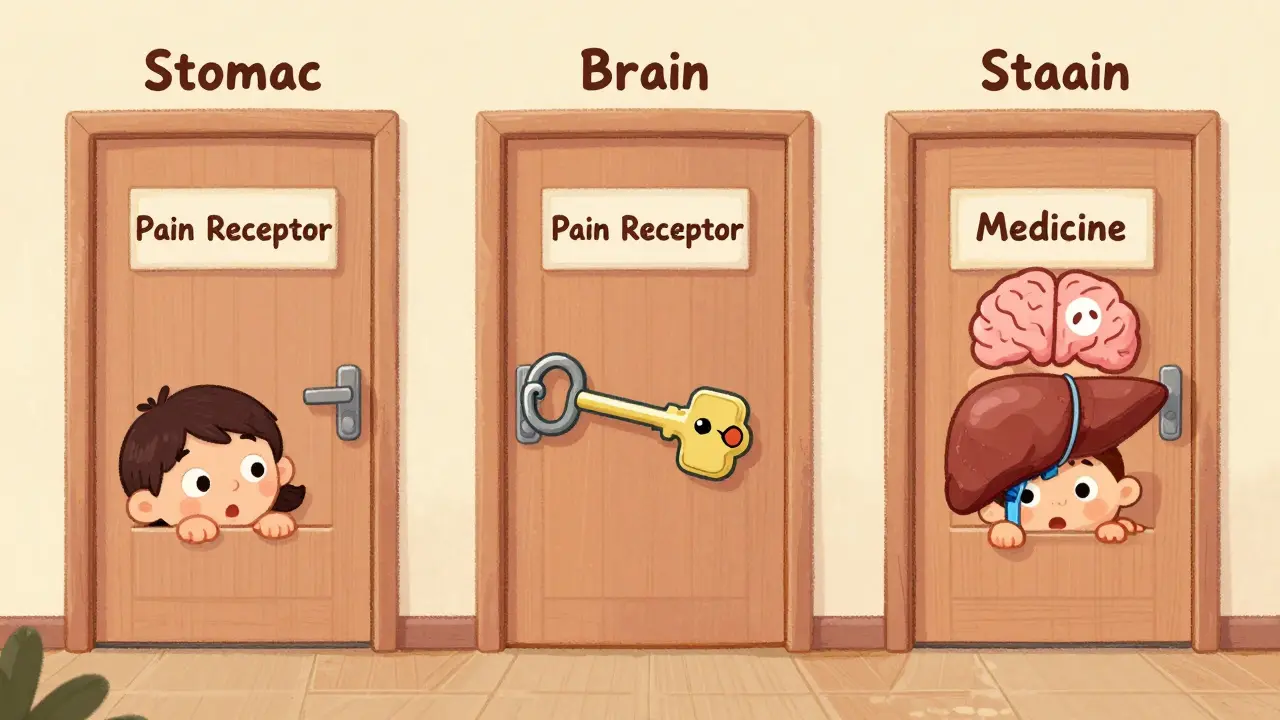
Side effects, or adverse drug reactions (ADRs), are unwanted effects that happen alongside the intended benefit of a medicine. The FDA defines them as any response to a drug that is noxious, unintended, and occurs at normal doses. Not all side effects are dangerous - some are mild, like dry mouth from antihistamines. Others can be life-threatening, like liver failure from certain antibiotics. But here’s the key: 75-80% of them are predictable. That means scientists understand exactly how and why they happen.Think of it this way: drugs are like keys. They’re designed to fit into one specific lock - say, a receptor in the brain that controls pain. But sometimes, the key doesn’t just open one lock. It can twist open others nearby. That’s how a drug meant to treat depression ends up causing weight gain or sexual dysfunction. It’s not broken. It’s just not perfectly selective.
How Your Body Processes Drugs: Pharmacokinetics
Before a drug can work, your body has to absorb it, move it around, break it down, and get rid of it. This whole process is called pharmacokinetics. And your genes play a huge role in how well it works.For example, the enzyme CYP2D6 breaks down more than 25% of common medications, including codeine, antidepressants, and beta-blockers. About 5-10% of people of European descent have a genetic variation that makes this enzyme work very slowly. These people are called “poor metabolizers.” When they take codeine, their bodies can’t convert it to morphine properly - so it doesn’t relieve pain. But in others, the enzyme works too fast, turning codeine into morphine too quickly, which can cause dangerous breathing problems.
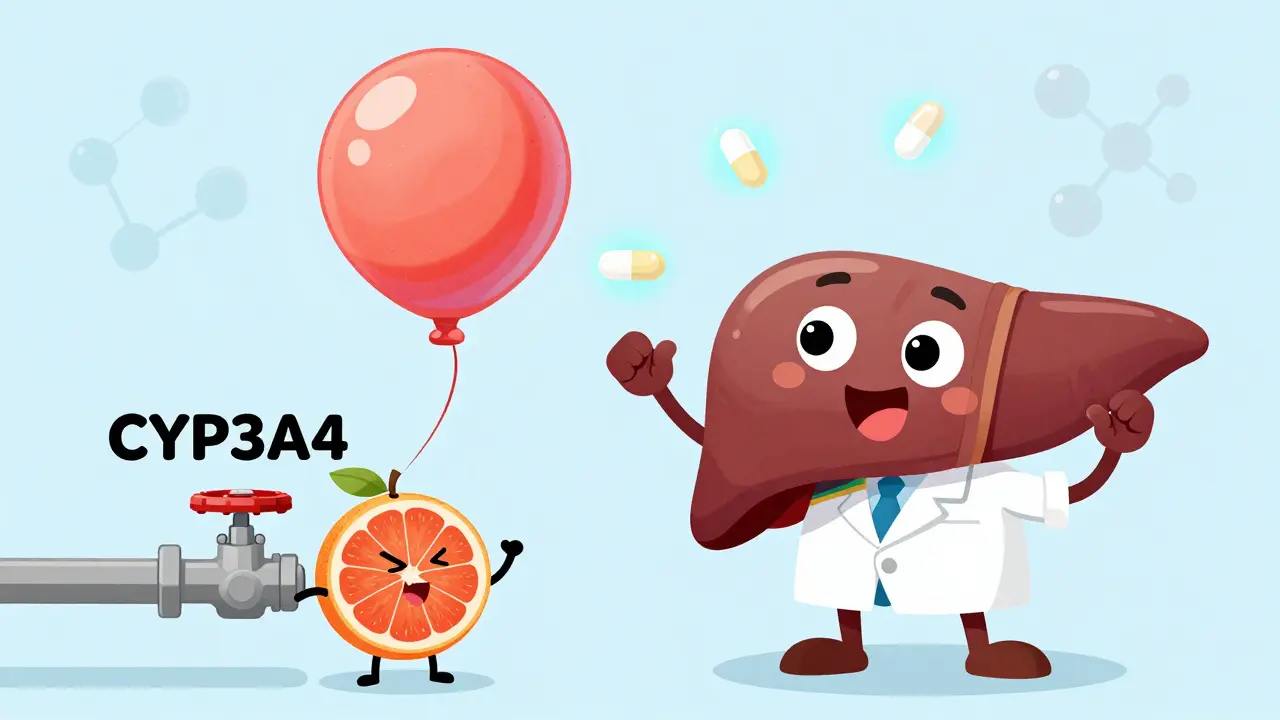
Then there’s the liver, which handles most drug metabolism. Some drugs force the liver to work overtime, while others block its ability to process other medications. Grapefruit juice is a classic example. It shuts down CYP3A4, a liver enzyme that breaks down drugs like felodipine (a blood pressure med). When you drink grapefruit juice with felodipine, the drug builds up in your blood - sometimes by 260%. That can drop your blood pressure so low you pass out.
Off-Target Effects: When Drugs Hit the Wrong Target
The biggest reason drugs cause side effects is because they don’t just act on one place. They act on many. This is called off-target toxicity.Take NSAIDs like ibuprofen or naproxen. They’re designed to block COX-2, an enzyme that causes inflammation and pain. But they also block COX-1, which protects your stomach lining by producing mucus and reducing acid. Without that protection, up to 30% of regular users develop stomach ulcers. That’s not a flaw in the drug - it’s a trade-off built into its chemistry.
Another example is haloperidol, an antipsychotic. It works by blocking dopamine receptors in the brain to reduce hallucinations. But dopamine receptors are also in the basal ganglia, which control movement. When haloperidol hits those receptors, it causes tremors, stiffness, and involuntary movements in 30-50% of patients. This isn’t rare. It’s expected.
Even more surprising: some drugs affect cell membranes themselves. A 2021 study from Weill Cornell Medicine showed that drugs that interact with the fatty layer surrounding cells - like antibiotics or anesthetics - can change the membrane’s thickness or flexibility. That, in turn, messes with proteins embedded in the membrane, even if those proteins aren’t the drug’s intended target. This explains why some drugs cause weird, multi-system side effects that don’t make sense at first glance.
Immune Reactions: When Your Body Turns Against the Drug
About 20-25% of side effects are unpredictable and tied to your immune system. These aren’t side effects in the traditional sense - they’re allergic or hypersensitivity reactions.Type I reactions are the most dangerous. They happen fast - within minutes - and involve IgE antibodies. Penicillin is the classic example. About 1 in 10,000 people who take it will have anaphylaxis: swelling, trouble breathing, and a sudden drop in blood pressure. It’s rare, but deadly if not treated immediately.
Type IV reactions are slower. They’re caused by T-cells and can show up days or weeks after taking the drug. Stevens-Johnson Syndrome, a severe skin reaction, falls into this category. It’s rare - only 1-6 cases per million people per year - but it’s most often linked to allopurinol, sulfonamides, or seizure meds like carbamazepine. People with the HLA-B*57:01 gene variant have a 50-100 times higher risk of reacting badly to abacavir, an HIV drug. That’s why doctors now test for this gene before prescribing it. The result? Hypersensitivity reactions have dropped from 5-8% to under 0.5%.
Then there are pseudoallergic reactions - things that look like allergies but aren’t. Vancomycin flushing syndrome, for instance, causes redness, itching, and low blood pressure in 10-15% of patients. But it’s not immune-driven. The drug directly triggers mast cells to release histamine. It’s not an allergy. It’s a direct chemical effect.
Drug Interactions: The Hidden Danger of Multiple Medications
The more pills you take, the higher your risk. That’s not just a warning on the label - it’s biology.Rifampicin, an antibiotic used for tuberculosis, speeds up the breakdown of other drugs by activating a protein called P-glycoprotein. When taken with digoxin (a heart medication), it can reduce digoxin levels by 30-50%. That means the heart drug stops working. Patients can end up in heart failure.
NSAIDs and methotrexate (used for arthritis and cancer) are another dangerous combo. NSAIDs reduce blood flow to the kidneys. That slows down how fast methotrexate gets cleared. The result? Toxic buildup that can crash your bone marrow. One study found this interaction caused life-threatening toxicity in 1 in 20 patients on both drugs.
Older adults are especially vulnerable. About 6-7% of hospital admissions in people over 65 are due to drug interactions. That number jumps sharply when someone takes five or more medications. It’s not that the drugs are bad. It’s that their combined effects are hard to predict without careful monitoring.

How Doctors Prevent Side Effects Today
We’re not just accepting side effects anymore. We’re learning how to stop them before they start.Pharmacogenomic testing is now standard for some drugs. Before prescribing abacavir, doctors check for HLA-B*57:01. Before giving clopidogrel (a blood thinner), they test for CYP2C19 mutations. Poor metabolizers get a different drug. No more treatment failures.
Therapeutic drug monitoring helps too. For drugs like digoxin or lithium, doctors measure blood levels to keep them in the safe zone. Digoxin, for example, is effective at 0.5-0.9 ng/mL. Above 1.2, it becomes toxic. Simple blood tests prevent hospitalizations.
Prophylactic用药 is another tool. If you’re on long-term NSAIDs and have a history of ulcers, your doctor will likely prescribe a proton pump inhibitor like omeprazole. Studies show this cuts ulcer risk by 70-80%.
And dose titration - starting low and going slow - works wonders for drugs like SSRIs. Up to 30% of people feel nauseous or dizzy at first. But if you start with a quarter of the full dose and increase slowly, those side effects drop dramatically.
The Future: AI, Prediction, and Safer Drugs
The next big leap isn’t just in how we use drugs - it’s in how we design them.The FDA’s Sentinel Initiative tracks side effects in real time across 300 million patient records. It caught that pioglitazone, a diabetes drug, doubled the risk of heart failure - something clinical trials missed because they were too small and too short.
Researchers at Weill Cornell are building computer models to predict which membrane proteins are most likely to be disrupted by a drug. If they succeed, drug companies could screen out dangerous compounds before they even reach human trials.
And AI is stepping in. A 2023 study in Nature Reviews Drug Discovery found that using machine learning to predict off-target effects early in development could reduce clinical trial failures due to toxicity by 25-30%. That’s billions of dollars saved - and more drugs reaching patients safely.
It’s not about avoiding medication. It’s about using it smarter. Side effects aren’t accidents. They’re signals. And now, we’re learning how to listen.
Why do some people get side effects and others don’t?
It comes down to genetics, age, liver and kidney function, and other medications. For example, people with certain gene variants like CYP2D6 poor metabolizers or HLA-B*57:01 are far more likely to react badly to specific drugs. Older adults process drugs slower, and taking multiple medications increases the chance of dangerous interactions.
Are all side effects dangerous?
No. Many side effects are mild and temporary - like dry mouth, drowsiness, or nausea. These often fade as your body adjusts. But some, like liver damage, severe rashes, or breathing trouble, are serious and need immediate medical attention. Always talk to your doctor if a side effect is new, worsening, or concerning.
Can I avoid side effects by stopping the drug?
Never stop a prescribed medication without talking to your doctor. Stopping suddenly can cause withdrawal symptoms or make your condition worse. If you’re having side effects, your doctor can adjust the dose, switch you to a different drug, or add a protective medication - like a stomach protector for NSAIDs.
Do natural supplements cause side effects too?
Yes. Many people assume “natural” means safe, but that’s not true. St. John’s wort can interfere with antidepressants, birth control, and blood thinners. Garlic and ginkgo can increase bleeding risk during surgery. Even vitamins like K or E can affect how your body responds to medications. Always tell your doctor what supplements you’re taking.
How do I know if a side effect is from my medication?
Track when symptoms started. If they began within days or weeks of starting a new drug, it’s likely connected. Note the timing, severity, and whether they improve after stopping the drug (under medical supervision). Your doctor can check databases like the FDA’s Adverse Event Reporting System or use pharmacogenomic tools to assess your risk.