Rivaroxaban is a direct oral anticoagulant (DOAC) that selectively inhibits factor Xa, preventing thrombin formation and reducing clot risk, approved for stroke prevention in non‑valvular atrial fibrillation and treatment of venous thromboembolism.
Why Stroke Prevention Matters
Every year, atrial fibrillation (AF) accounts for roughly 15% of all ischemic strokes in the United States. The chaotic rhythm lets blood pool in the atria, forming clots that can travel to the brain. Without anticoagulation, the five‑year stroke risk for a typical AF patient can exceed 20%.
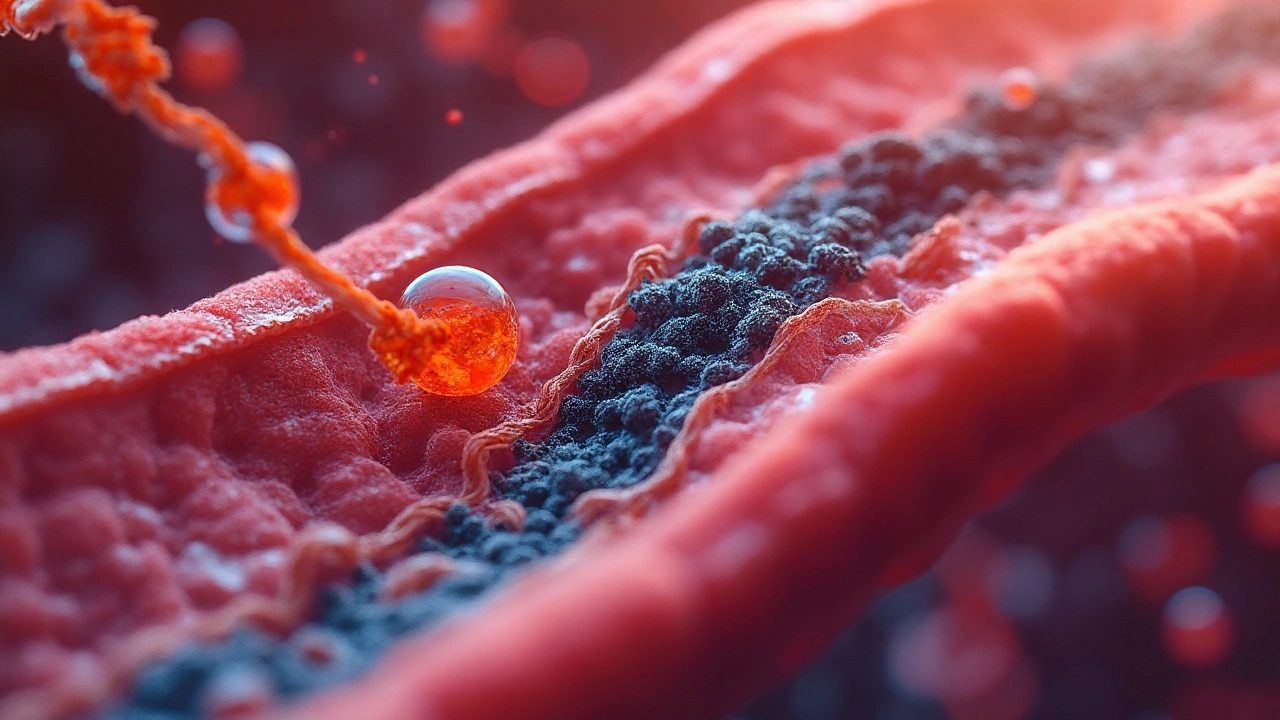
How Rivaroxaban Works
Rivaroxaban belongs to the class of factor Xa inhibitors agents that block the final common pathway of the coagulation cascade. By binding directly to factor Xa, it stops the conversion of prothrombin to thrombin, halting fibrin clot formation. Unlike older agents, it does not require routine lab monitoring because its pharmacokinetics are predictable.
Clinical Evidence Supporting Stroke Prevention
The landmark ROCKET‑AF trial enrolled 14,000 patients with NVAF and compared rivaroxaban 20mg once daily (15mg for CrCl 30-49mL/min) to warfarin (INR 2.0-3.0). Over a median 2‑year follow‑up, rivaroxaban demonstrated non‑inferior efficacy (1.7% vs 2.2% annual stroke/systemic embolism rate) and a statistically significant reduction in intracranial hemorrhage (0.4% vs 0.7%). Real‑world registries published by the American Heart Association in 2023 confirm similar outcomes across diverse ethnic groups.
Comparing Rivaroxaban with Other Anticoagulants
Patients often wonder how rivaroxaban stacks up against warfarin and other DOACs such as apixaban. The table below summarizes key differences.
| Attribute | Rivaroxaban | Warfarin | Apixaban |
|---|---|---|---|
| Mechanism | Factor Xa inhibitor | Vitamin K antagonist | Factor Xa inhibitor |
| Dosing Frequency | Once daily | Variable (dose adjusted to INR) | Twice daily |
| Monitoring | No routine labs | INR checks 2-4times/week initially | No routine labs |
| Food Interactions | Minimal | Many (e.g., leafy greens, alcohol) | Minimal |
| Renal Dose Adjustment | Yes, CrCl30‑49mL/min | None | Yes, CrCl15‑29mL/min |
| Major Bleeding Rate | 2.1%/yr | 3.4%/yr | 1.9%/yr |
Who Should Take Rivaroxaban?
Decision‑making begins with the CHA₂DS₂‑VASc score a risk stratification tool for stroke in AF patients. Patients scoring ≥2 (men) or ≥3 (women) are candidates for anticoagulation. At the same time, the HAS‑BLED score assesses bleeding risk based on hypertension, abnormal renal/liver function, stroke history, bleeding history, labile INR, elderly age, drugs/alcohol helps weigh safety.
Rivaroxaban is especially attractive for patients with unstable INR control, those who travel frequently, or individuals who prefer a single daily pill. However, patients with severe hepatic impairment (Child‑Pugh C) or creatinine clearance <30mL/min should avoid it.
Practical Dosing and Renal Considerations
The standard dose for stroke prevention is 20mg once daily with the evening meal. For moderate renal impairment (CrCl 30‑49mL/min), the dose drops to 15mg. The drug’s half‑life is about 5‑9hours, but the pharmacodynamic effect lasts 24hours, enabling once‑daily dosing.
Renal function should be checked at baseline and at least annually. In patients whose creatinine clearance declines below 30mL/min, clinicians should transition to an alternative agent or discontinue therapy.
Managing Bleeding Risks
While rivaroxaban reduces intracranial hemorrhage, gastrointestinal bleeding remains a concern. If a major bleed occurs, the specific reversal agent andexanet alfa a recombinant modified factor Xa protein that binds and neutralizes rivaroxaban is available, though costly. Supportive measures-cessation of the drug, mechanical compression, and transfusion if needed-are first‑line.
Patients should be counselled on recognizing warning signs such as persistent nosebleeds, melena, or hematuria, and instructed to seek urgent care.
Special Populations and Emerging Data
Recent sub‑analyses of the ROCKET‑AF and COMPASS trials indicate that rivaroxaban benefits extend to patients with stable coronary artery disease when combined with low‑dose aspirin, reducing the composite endpoint of cardiovascular death, stroke, or myocardial infarction. Nevertheless, the combination raises bleeding risk, so shared decision‑making is vital.
In patients aged ≥80years, real‑world data from the FDA’s Sentinel system (2024) show comparable stroke reduction with a modest increase in major bleeding versus younger cohorts, underscoring the need for individualized dosing and vigilant monitoring.
Bottom Line: Putting It All Together
Rivaroxaban offers a convenient, once‑daily, lab‑free alternative to warfarin for stroke prevention in AF, with solid trial‑backed efficacy and a favorable bleeding profile, particularly for intracranial events. Its success hinges on proper patient selection, renal assessment, and education about bleeding signs. When used appropriately, it can dramatically cut stroke risk while simplifying the patient’s daily routine.
Frequently Asked Questions
Can I switch from warfarin to rivaroxaban?
Yes. The typical approach is to stop warfarin and start rivaroxaban once the INR falls below 2.0. Overlap isn’t needed because rivaroxaban acts quickly.
Do I need regular blood tests while on rivaroxaban?
Routine coagulation tests aren’t required. A baseline kidney panel is recommended, then annually or sooner if you develop kidney disease.
What happens if I miss a dose?
Take the missed tablet as soon as you remember, as long as it’s within 12hours of the scheduled time. If it’s later, skip it and resume your regular schedule. Doubling up isn’t advised.
Is rivaroxaban safe during pregnancy?
No. Rivaroxaban is classified as pregnancy categoryX; it can cross the placenta and increase fetal bleeding risk. Warfarin or low‑molecular‑weight heparin are preferred in pregnant patients with AF.
How does rivaroxaban compare to apixaban for stroke prevention?
Both are factor Xa inhibitors with similar efficacy. Apixaban has a slightly lower major‑bleed rate (1.9% vs 2.1% per year) and is dosed twice daily, which some patients find less convenient. Choice often depends on renal function, dosing preference, and cost.
Can I take rivaroxaban with aspirin?
In selected patients with coronary artery disease, low‑dose aspirin (81mg) plus rivaroxaban 2.5mg twice daily has shown cardiovascular benefit, but the bleeding risk rises. Discuss the balance with your cardiologist.


They’re lying to you. Rivaroxaban? It’s just a front for Big Pharma’s real agenda - they want you dependent on pills so they can charge you $500 a month while the FDA looks the other way. I’ve seen the leaked emails. They know it causes hidden liver damage that shows up YEARS later. They don’t care if you bleed out in your sleep - as long as the stock price stays up. #RivaroxabanCoverUp
Look, I get it - we all want the easy fix, right? One pill a day, no blood tests, no hassle. But let’s be real - we’re trading one kind of control for another. Warfarin was a pain, sure, but at least you knew where you stood. With rivaroxaban? You’re flying blind. And don’t get me started on how they market this like it’s a magic bullet while ignoring the fact that half the people taking it don’t even know what atrial fibrillation is. It’s not about convenience - it’s about corporate convenience. We’re being sold a dream wrapped in a prescription bottle. And yeah, I’m not mad, I’m just disappointed.
Let’s be clear: rivaroxaban is NOT for everyone. The HAS-BLED score exists for a reason - if you’re drinking, have uncontrolled HTN, or are over 75, you’re playing Russian roulette. And yet, doctors still prescribe it like candy. I’ve seen patients on it who can’t even pronounce ‘anticoagulant.’ It’s irresponsible. And no - ‘minimal food interactions’ doesn’t mean ‘no consequences.’ The liver doesn’t care how convenient it is. 🚨
While the clinical efficacy of rivaroxaban, as demonstrated in the ROCKET-AF trial, is statistically non-inferior to warfarin, one must critically evaluate the long-term pharmacoeconomic implications and the absence of a reversal agent in many clinical settings. The reduction in intracranial hemorrhage, though statistically significant, does not mitigate the elevated risk of gastrointestinal bleeding - a complication that remains underreported in real-world registries. Furthermore, the absence of routine monitoring constitutes a paradigmatic shift in clinical governance, one that prioritizes patient compliance over clinical vigilance. This is not progress - it is commodification of care.
Wait - did you just say ‘creatinine clearance’ and then cut off mid-sentence? That’s it? That’s your whole article? You left out the most critical part - the renal dosing thresholds for patients with CrCl <15 mL/min? And you didn’t even mention the black box warning for spinal/epidural hematomas in patients on concurrent NSAIDs? This isn’t patient education - it’s negligence. Fix it. Immediately. 🙄
So basically, it’s just another drug that’s ‘better’ until someone dies. 😑
As someone from India where warfarin is still the go-to because of cost, I’ve seen both sides. Rivaroxaban is great if you can afford it - no more weekly INR trips, no more cabbage avoidance. But in rural clinics, we don’t have access to reversal agents or emergency labs. So yes, it’s safer on paper - but in practice? It’s a luxury. Hope things change soon.