Why Therapeutic Drug Monitoring Matters for Generic NTIs
Not all generic drugs are created equal-especially when it comes to NTI drugs. These are narrow therapeutic index medications where even a small change in blood concentration can mean the difference between effective treatment and dangerous toxicity. Think of it like driving a car with no speedometer: you might think you’re going 55 mph, but if your speedometer is off by just 10%, you could be going 60 or 50-either way, you’re at risk. That’s exactly what happens when patients switch from brand-name NTI drugs to generics without proper monitoring.
NTI drugs include medications like warfarin, levothyroxine, phenytoin, cyclosporine, and certain antiretrovirals. For these, the gap between a therapeutic dose and a toxic one is razor-thin. A 10% drop in concentration might make the drug useless. A 10% rise could cause organ damage, seizures, or even death. The FDA allows generics to vary by up to 20% in bioavailability compared to the brand-name version. That’s acceptable for most drugs-but not for NTIs. That’s where therapeutic drug monitoring (TDM) steps in.
What Is Therapeutic Drug Monitoring (TDM)?
TDM isn’t just checking a drug level in the blood. It’s a process: draw blood at the right time, measure the exact concentration, compare it to a known target range, and adjust the dose if needed. It’s not a one-time test. It’s repeated over time, especially after a dose change, a new medication, or a switch to a generic version.
For example, if a patient takes brand-name cyclosporine and then switches to a generic, their blood level might drop from 150 ng/mL to 110 ng/mL. That’s still within the 20% FDA tolerance-but it’s now below the therapeutic window for transplant rejection prevention. Without TDM, the doctor might assume the patient isn’t taking the drug, not realizing the generic is simply less reliably absorbed. TDM catches that gap.
The key to TDM is having accurate, validated lab tests and knowing the right target range for each drug in each patient. For some drugs, like phenytoin, the target range is 10-20 mcg/mL. Go below 10, and seizures return. Go above 20, and you risk tremors, confusion, or coma. There’s no room for guesswork.
Why Generic NTIs Are Riskier Than You Think
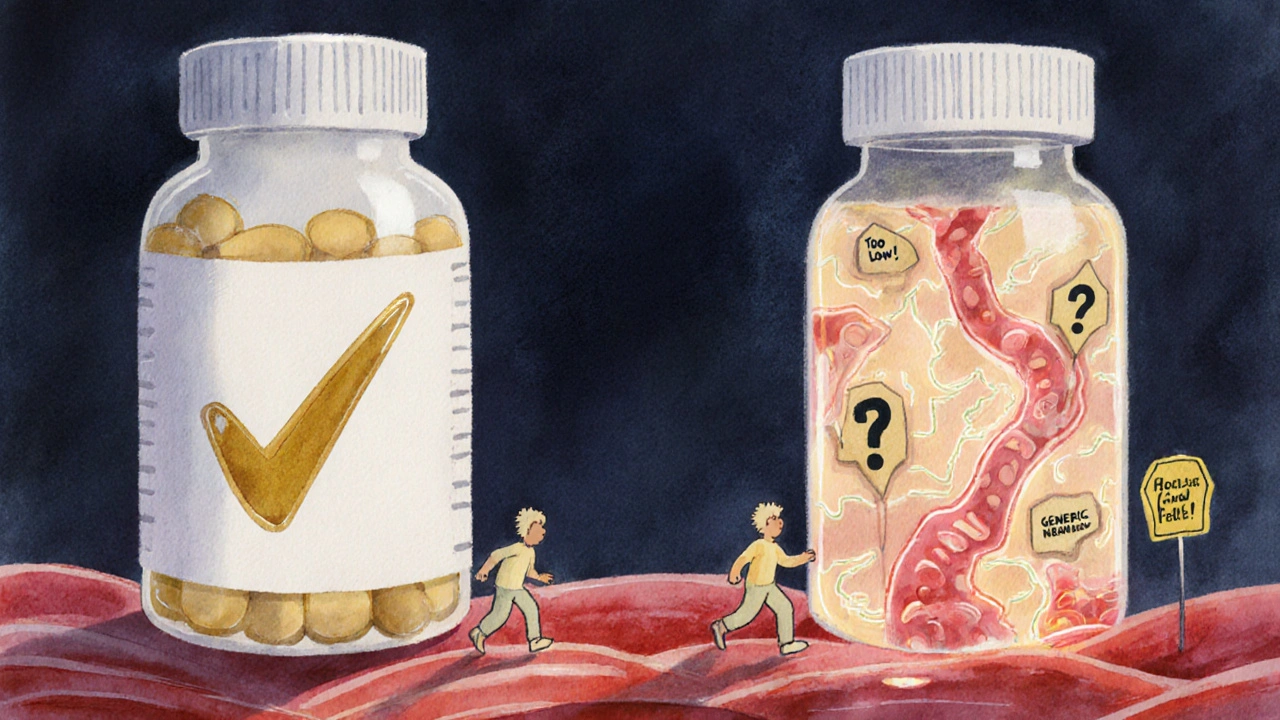
Many patients assume generics are exact copies. They’re not. They contain the same active ingredient, yes-but fillers, coatings, and manufacturing processes differ. Those differences can affect how quickly the drug dissolves, how well it’s absorbed, and how long it stays in the bloodstream.
One 2023 study in the Journal of Clinical Pharmacy and Therapeutics tracked 87 patients switched from brand to generic levothyroxine. Nearly 30% had a significant change in TSH levels within 6 weeks. Some needed dose adjustments. Others developed symptoms of hypothyroidism-fatigue, weight gain, depression-because their bodies weren’t getting enough hormone.
In transplant patients, switching generics can be life-threatening. A 2022 report from the Mayo Clinic showed that 12% of kidney transplant patients on generic cyclosporine experienced acute rejection within 90 days of switching. In every case, TDM revealed drug levels had fallen below the minimum effective threshold. The patients weren’t noncompliant. The generic was just less predictable.
This isn’t about quality control. It’s about variability. Even FDA-approved generics can behave differently in different people. And when you’re dealing with a drug where 10% can kill you, variability is a problem.
When TDM Is Essential-And When It’s Not
TDM isn’t needed for every drug. It’s only useful when:
- The drug has a narrow therapeutic index
- There’s wide variation in how people absorb or metabolize it
- A blood level reliably predicts effectiveness or toxicity
For drugs like statins, antibiotics, or antidepressants, TDM isn’t practical-or helpful. But for NTIs? It’s often critical.
Here’s a quick guide:
| Drug Class | Examples | Why TDM Matters |
|---|---|---|
| Immunosuppressants | Cyclosporine, tacrolimus | Too low = organ rejection. Too high = kidney damage. |
| Antiepileptics | Phenytoin, valproic acid | Small changes cause seizures or toxicity. |
| Anticoagulants | Warfarin | INR must stay in range. Generic switching can alter response. |
| Thyroid Hormones | Levothyroxine | Even minor absorption changes affect TSH levels. |
| Antiretrovirals | Protease inhibitors (e.g., lopinavir) | Generic versions may have lower bioavailability in some patients. |
For drugs like NRTIs (e.g., tenofovir, emtricitabine), TDM doesn’t work. They’re prodrugs that activate inside cells, not in the blood. So checking plasma levels tells you nothing. But for protease inhibitors and NNRTIs? Blood levels matter a lot. That’s why TDM is still used in HIV care for certain drugs-even though it’s not routine.
Real-World Consequences of Skipping TDM
There’s a story from a Phoenix clinic in 2024. A 58-year-old man with a heart transplant was switched to a generic tacrolimus after his insurance denied the brand. He felt fine. His doctor saw no reason to check levels. Three months later, he was rushed to the hospital with acute kidney failure. His tacrolimus level was 3.2 ng/mL-well below the 5-10 ng/mL target. The generic version had lower absorption in his gut. He’d been underdosed for weeks. He survived, but lost 30% of his kidney function.
On the other side, a 62-year-old woman on generic phenytoin developed tremors and slurred speech. Her level was 28 mcg/mL-above the toxic threshold. She’d been stable on brand-name for years. The generic had higher bioavailability. TDM caught it before she had a seizure.
These aren’t rare cases. A 2023 analysis of U.S. hospital data found that 1 in 12 patients on generic NTIs experienced a clinically significant event within 90 days of switching. TDM could have prevented half of them.
How TDM Works in Practice
Getting TDM done isn’t complicated, but it’s not automatic. Here’s how it works:
- When switching to a generic NTI, schedule a blood draw 2-4 weeks after the change.
- Draw the blood at the right time-usually just before the next dose (trough level).
- Use a lab with validated assays. Not all labs can measure NTI drugs accurately.
- Compare the result to the established therapeutic range for that drug in that patient.
- If the level is out of range, adjust the dose and retest in 1-2 weeks.
Some clinics do this as standard practice. Others wait for a problem to happen. The difference? One saves lives. The other reacts to crises.
Turnaround time matters too. In public hospitals, results can take 10-14 days. In private labs, you can get them in 48 hours. For high-risk patients, that delay can be dangerous. That’s why some specialists keep a small stock of brand-name drugs on hand for patients who can’t wait.
Cost, Access, and Barriers
TDM isn’t cheap. A single test can cost $150-$400. Insurance often won’t cover it unless there’s a clear medical reason-like a recent switch, kidney problems, or drug interactions.
Many primary care doctors don’t know when to order it. Pharmacists might suggest it, but if the prescriber doesn’t understand the value, it gets ignored. There’s also a lack of standardized target ranges for some generics. What’s “normal” for one brand might not be for another.
But the cost of not doing TDM? Higher. Hospitalizations, organ transplants gone wrong, emergency room visits-those cost thousands. TDM is a preventive tool. It’s like checking your brakes before a long drive. You don’t wait until you’re skidding to fix them.

What Patients Should Do
If you’re on an NTI drug-especially if you’ve recently switched to a generic-ask your doctor:
- Is this a narrow therapeutic index drug?
- Has my blood level been checked since I switched?
- Can we do a TDM test now?
- What’s my target range?
Don’t assume you’re fine because you feel okay. Symptoms often appear after damage is already done. And if your doctor says, “We don’t do that here,” ask for a referral to a specialist-pharmacists, infectious disease doctors, or transplant clinics often have more experience with TDM.
The Future of TDM and Generic NTIs
Regulators are starting to pay attention. The FDA now recommends TDM for certain NTIs when switching generics. The European Medicines Agency has issued similar guidance. Some states in the U.S. are passing laws requiring pharmacists to notify patients when switching NTIs.
But the real change will come from awareness. More doctors need to know that generics aren’t always interchangeable for NTIs. More labs need to offer reliable assays. More patients need to ask the right questions.
For now, if you’re on a drug where a small change can hurt you-don’t wait for a crisis. Ask for a blood test. It’s not about distrust in generics. It’s about making sure they work for you.
What does NTI stand for in drug terms?
NTI stands for Narrow Therapeutic Index. It means the difference between a safe, effective dose and a toxic dose is very small. Even slight changes in blood levels can lead to treatment failure or serious side effects. Examples include warfarin, levothyroxine, phenytoin, and cyclosporine.
Why is TDM not used for all generic drugs?
TDM is only useful for drugs where blood levels directly predict effectiveness or toxicity, and where there’s high variability between individuals. For most drugs-like antibiotics or blood pressure meds-the body handles them consistently enough that routine monitoring isn’t needed. But for NTIs, that consistency can’t be assumed.
Can I switch back to the brand-name drug if I have problems with the generic?
Yes. If you experience unexplained side effects or loss of effectiveness after switching to a generic NTI, talk to your doctor. They can request a prior authorization from your insurance to return to the brand-name version. TDM results can help support this request by showing your drug levels are outside the safe range.
How often should TDM be done for NTI drugs?
After switching to a new generic, test within 2-4 weeks. Then repeat if your dose changes, you start or stop another medication, or you develop new symptoms. Once stable, testing every 6-12 months is often enough-unless you have liver or kidney issues, which can alter drug levels.
Are there any risks to doing TDM?
The main risk is delay in results-if it takes two weeks to get your levels back, and your drug level is dangerously low or high, you could be at risk during that time. Also, some patients may over-rely on TDM and ignore other factors like adherence or diet. TDM is a tool, not a replacement for good communication with your care team.
Next Steps for Patients and Providers
If you’re a patient on an NTI drug: make a list of all your medications and note which ones are NTIs. Ask your pharmacist if any recent switches involved generics. Schedule a TDM test if you’ve switched in the last 3 months.
If you’re a provider: add a checklist for NTI drugs in your EHR. Flag any patient who switches generics for an NTI. Don’t assume stability. Test early, test often, and don’t wait for a crisis to act.
For everyone: remember this-when safety margins are thin, precision matters. TDM isn’t fancy science. It’s basic medicine. And for patients on generic NTIs, it might be the only thing standing between them and harm.