When a patient walks in with shortness of breath, fatigue, or swollen ankles, the question isn’t just "Is it heart failure?" - it’s "Can I rule it out quickly, safely, and without spending $3,000 on an echocardiogram?" That’s where NT-proBNP blood testing comes in. It’s not just another lab order. For clinicians, it’s the fastest, most reliable way to cut through the noise and make decisions with confidence.
Why NT-proBNP? It’s Not Just Another Biomarker
NT-proBNP stands for N-terminal pro-B-type natriuretic peptide. It’s a protein fragment released by the heart when its ventricles are stretched from too much pressure - the exact moment heart failure starts to develop. Unlike symptoms that can mimic lung disease, kidney problems, or even anxiety, NT-proBNP gives you an objective number. And that number has been validated in over 28 years of outcome data. The test measures the inactive part of the hormone that the heart produces in response to stress. It’s more stable than its cousin BNP, which breaks down quickly in the blood. NT-proBNP lasts longer, so even if a sample sits for a few hours before testing, the result won’t drift. That’s why 68% of U.S. hospitals now prefer NT-proBNP over BNP for heart failure evaluation.When to Order: The 5 Clear Clinical Scenarios
You don’t order this test for everyone. But when you do, it changes everything. Here are the five situations where NT-proBNP is a game-changer:- Acute dyspnea in the ER - A 74-year-old with sudden trouble breathing. Is it heart failure? COPD? A pulmonary embolism? NT-proBNP under 300 pg/mL rules out heart failure with 98% accuracy. That’s enough to avoid hospital admission, unnecessary imaging, and days of waiting.
- Chronic heart failure monitoring - If a patient is on diuretics or ACE inhibitors, a rising NT-proBNP level can signal worsening function before they even feel worse. A 20% increase over baseline often means it’s time to adjust meds - not wait for edema to return.
- Screening in high-risk patients - Diabetics, those with hypertension, or a history of heart attack. These patients often don’t have classic symptoms. A baseline NT-proBNP helps catch early remodeling. Levels above 450 pg/mL in someone under 50 should trigger an echo.
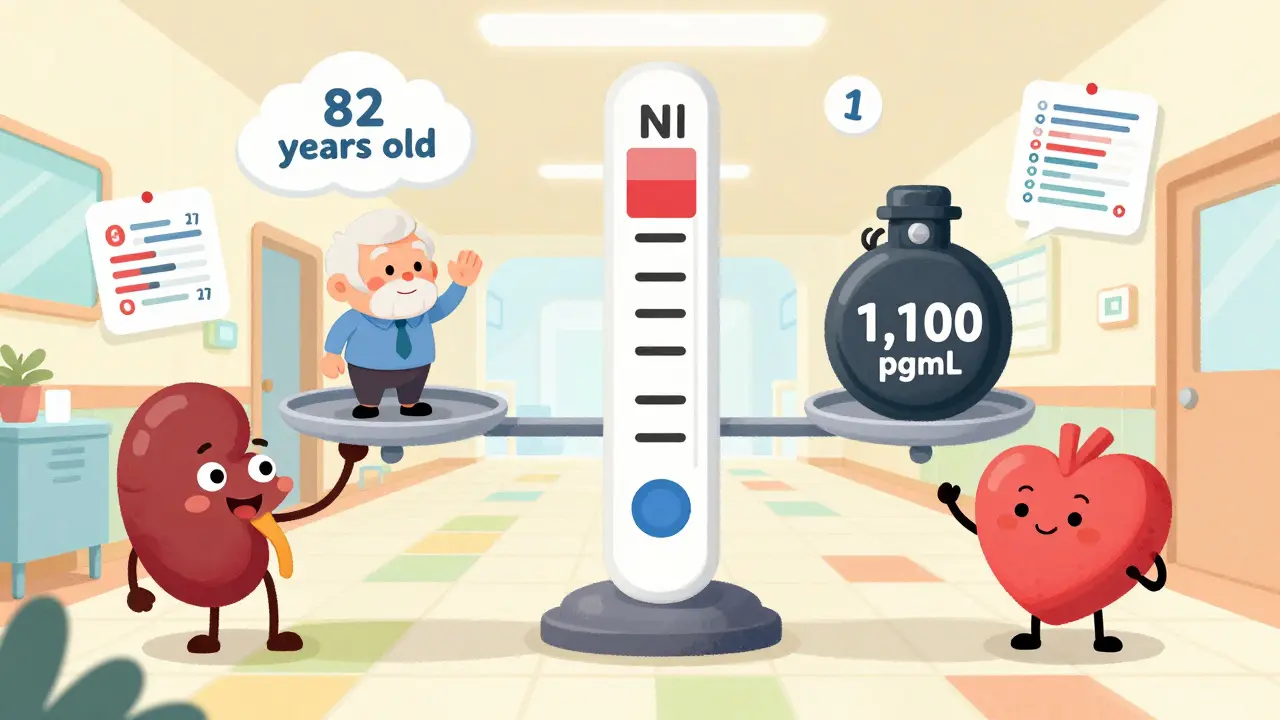
- Unclear heart failure in elderly patients - A 82-year-old with mild swelling and fatigue? It’s easy to blame aging. But if NT-proBNP is 1,100 pg/mL, that’s not just "getting older." It’s likely heart failure - even if the echocardiogram looks okay.
- Post-acute coronary syndrome risk stratification - Starting in 2024, new guidelines recommend NT-proBNP testing after a heart attack. High levels predict higher risk of death or rehospitalization. That’s not just diagnosis - it’s prognosis.
Understanding the Numbers: Age, Kidneys, and Obesity
The biggest mistake clinicians make? Treating NT-proBNP like a single cutoff for everyone. It’s not. The number means different things depending on who you’re looking at.- Age matters - Levels rise naturally with age. For someone under 50, anything over 450 pg/mL is suspicious. For someone over 75, 900 pg/mL is the new upper limit of normal. Ignore this, and you’ll overdiagnose heart failure in the elderly.
- Kidney disease changes everything - If a patient has stage 3 or 4 chronic kidney disease, NT-proBNP levels can be 28-40% higher than normal - even without heart failure. Use the adjusted ESC cutoff: rule out heart failure at <1,200 pg/mL in advanced CKD.
- Obesity lowers the signal - Fat tissue absorbs natriuretic peptides. For every 5-point increase in BMI, levels drop 25-30%. So if a 120 kg patient has a level of 400 pg/mL, that’s actually high for them. Don’t dismiss it just because it’s "below normal."
What NT-proBNP Can’t Do
It’s powerful - but not magic. Here’s where it fails:- It doesn’t tell you the cause - A high level means the heart is stressed, but not why. Is it from hypertension? Valvular disease? Arrhythmia? You still need the clinical picture, echo, and history.
- It’s not for screening healthy people - Medicare data shows 18% of tests are ordered in asymptomatic patients. That’s wasteful. No one benefits from testing a 45-year-old with no symptoms and normal blood pressure.
- It can’t replace physical exams - A jugular venous distention, crackles in the lungs, or a third heart sound still matter. NT-proBNP supports, doesn’t replace, clinical judgment.
Real-World Impact: What Happens When You Use It Right
In a 2022 UK national audit, hospitals that used NT-proBNP as a first-line test for suspected heart failure reduced unnecessary echocardiograms by 19%. That’s not just saving money - it’s reducing patient anxiety and freeing up scarce imaging slots. One cardiologist in Boston told me about a patient who came in with chest tightness after a flu. Her NT-proBNP was 120 pg/mL. No heart failure. No hospital stay. No stress test. Just rest and fluids. She walked out the same day. Another case: a 78-year-old with atrial fibrillation and stage 3 CKD. His NT-proBNP was 850 pg/mL. Was it heart failure? Or just aging and kidney disease? He didn’t meet the adjusted cutoff for rule-out (<1,200 pg/mL), so he got an echo. Turns out, his ejection fraction was 30%. He started on guideline-directed therapy. He’s been stable for 18 months.
Getting the Test Right: Logistics and Pitfalls
The test itself is simple. One tube of serum, 1 mL. No fasting needed. Results come back in under an hour in most hospitals. Roche’s Elecsys assay is the most common - used in 73% of U.S. labs. But here’s where things go wrong:- Wrong tube - Serum separator tubes only. If you use EDTA or heparin, the result is invalid.
- Delayed processing - While stable for 72 hours at 4°C, samples left at room temperature for more than 6 hours can degrade. Don’t let phlebotomy delays compromise results.
- Ignoring comorbidities - The most common error isn’t technical - it’s interpretive. A 90-year-old with atrial fibrillation and mild renal impairment? Don’t panic at 700 pg/mL. Adjust the cutoff. Consult the guidelines.
The Future: Point-of-Care and Beyond
In 2023, the FDA cleared the first point-of-care NT-proBNP device - Roche’s Cobas h 232. It delivers results in 12 minutes, with 94.7% accuracy compared to central lab testing. Now, emergency departments can know within 15 minutes whether a patient can go home or needs admission. The 2024 ACC/AHA/HFSA guidelines will expand its use to include risk stratification after heart attacks. Studies like VICTORIA show that a drop in NT-proBNP after treatment predicts lower risk of death. That’s moving the test from diagnosis to monitoring therapy response.Bottom Line: Don’t Overuse It - But Don’t Underuse It Either
NT-proBNP isn’t a screening tool for the general population. But in the right hands, at the right time, it’s one of the most valuable tests in medicine. It prevents unnecessary hospitalizations. It shortens emergency department stays. It helps patients avoid invasive tests. The key is knowing when to order it - and how to read it. Use age-adjusted and kidney-adjusted cutoffs. Combine it with clinical signs. Don’t treat it as a standalone answer. When used correctly, NT-proBNP doesn’t just answer a question - it changes the trajectory of care.What is a normal NT-proBNP level?
There’s no single "normal" level - it depends on age and kidney function. For patients under 50, levels below 450 pg/mL typically rule out heart failure. For those 50-75, the cutoff is 900 pg/mL. For patients over 75, levels below 1,800 pg/mL are often considered normal. In patients with advanced kidney disease (CKD stage 3-5), use a higher rule-out threshold of <1,200 pg/mL.
Can NT-proBNP be elevated without heart failure?
Yes. NT-proBNP can rise in conditions like chronic kidney disease, atrial fibrillation, severe lung disease, or even after major surgery. It reflects cardiac stress, not just heart failure. That’s why context matters - always interpret results alongside symptoms, physical exam, and other tests.
How often should NT-proBNP be repeated?
In acute settings, a single test is usually enough to rule in or rule out heart failure. For chronic heart failure patients, repeat every 3-6 months if stable. If symptoms worsen or medications change, retest within 2-4 weeks. A rising trend is more telling than a single value.
Is NT-proBNP better than BNP?
For most clinical purposes, yes. NT-proBNP is more stable in blood samples, has a longer half-life, and shows slightly higher diagnostic accuracy in large studies. It’s also less affected by medication changes. Most U.S. labs now prefer NT-proBNP, and guidelines favor it for initial testing.
Can obesity affect NT-proBNP results?
Yes. Fat tissue absorbs natriuretic peptides, so obese patients often have lower NT-proBNP levels - sometimes 25-30% lower than expected for their heart condition. A level that looks "normal" in a 120 kg patient might actually be elevated. Never rely solely on standard cutoffs in obesity.
What if NT-proBNP is normal but I still suspect heart failure?
If NT-proBNP is below the rule-out threshold (e.g., <300 pg/mL in acute settings), heart failure is extremely unlikely. If clinical suspicion remains high, consider other causes - pulmonary hypertension, restrictive cardiomyopathy, or even non-cardiac issues like severe anemia or thyroid disease. An echocardiogram may still be warranted, but it’s no longer a first-line reflex.


NT-proBNP is one of those tests that should be in every ER’s default panel. I’ve seen too many patients get lost in the shuffle because everyone’s afraid to order imaging. This thing saves time, money, and stress. No brainer.
Let’s be real - we’re just replacing clinical judgment with a number that rises with age, kidney function, and bad coffee. Sure, it’s ‘validated,’ but so was bloodletting. The real question is whether we’re using it to guide care or just to justify our own uncertainty.
I appreciate how you laid out the five scenarios. I’ve used this test in the clinic for chronic HF patients and it’s been a game-changer. One guy’s levels crept up 22% over three weeks - we adjusted his diuretic, and he avoided a readmission. Simple, cheap, effective.
The post contains multiple grammatical inconsistencies, including improper punctuation and run-on sentences. Furthermore, the assertion that NT-proBNP ‘rules out’ heart failure with 98% accuracy is misleading without specifying the negative predictive value in context of pretest probability. Medical communication must be precise, not performative.
You think 450 is the cutoff for under 50? That’s what the guidelines say, but real-world data from the 2023 JACC meta-analysis shows 380 is more accurate in obese patients. And you didn’t even mention BMI-adjusted thresholds. Classic textbook thinking. You’re missing half the picture.
NT-proBNP is overused. If you’re ordering it for every old person with swollen ankles you’re just creating noise. I’ve seen labs bill for it three times in one week on the same patient. It’s not a screening tool. It’s a diagnostic tool. Stop turning it into a routine.
From my time working in rural India, I’ve seen how this test changes outcomes where echo machines are rare or broken. We don’t have fancy tech but we have blood draws. NT-proBNP lets us treat heart failure without a cardiologist on site. It’s not perfect but it’s the best tool we’ve got.
It’s infuriating how clinicians treat this test like a magic wand. You can’t just look at the number and say ‘heart failure’ - you need to integrate it with history, physical, and context. And yet, every intern I’ve trained thinks a high NT-proBNP means they’ve ‘solved’ the case. We’re turning medicine into a multiple choice quiz.
This test is the unsung hero of cardiology - the quiet ninja of the lab. It doesn’t shout like an MRI or demand a full-day slot like an echo. It just sits there, steady and reliable, whispering the truth in pg/mL. If labs had Oscars, NT-proBNP would win Best Supporting Actor.
I’ve had patients come in with NT-proBNP at 1800 and no symptoms. Then the echo shows mild LVH. Turns out they’ve had undiagnosed HTN for 15 years. So yeah, sometimes the number tells you what the patient won’t admit.
Every time I see someone say ‘just order NT-proBNP’ I feel like we’re losing the soul of medicine. We used to listen. We used to feel the pulse, watch the jugular, hear the crackles. Now we just type a code into the computer and call it diagnosis. This isn’t progress. It’s surrender.