Bipolar Antidepressant Risk Calculator
This tool calculates your risk of mood switching (from depression to mania/hypomania) when taking antidepressants based on your specific bipolar disorder history. Your results will show your personalized risk percentage compared to the natural switch rate with mood stabilizers alone (10.7%).
For decades, doctors treated bipolar depression the same way they treated regular depression: with antidepressants. But the reality is far more complicated. In bipolar disorder, these medications don’t just lift mood-they can trigger mania, rapid cycling, or even suicidal episodes. This isn’t a rare side effect. It’s a well-documented risk that’s reshaping how psychiatrists approach treatment today.
Why Antidepressants Are Risky in Bipolar Disorder
Antidepressants work by boosting serotonin, norepinephrine, or dopamine. That’s fine for unipolar depression, where the brain’s mood circuits are simply underactive. But in bipolar disorder, those same circuits are unstable. A small nudge can push someone from deep depression into full-blown mania-or worse, a mixed state where they feel agitated, hopeless, and energized all at once.
Studies show that about 12% of people with bipolar disorder who take antidepressants experience a switch into mania or hypomania. That number jumps to 31% in real-world, retrospective studies where patients aren’t tightly monitored. For comparison, the natural switch rate with mood stabilizers alone is around 10.7%. So antidepressants aren’t just adding benefit-they’re adding danger.
The risk isn’t the same for everyone. People with Bipolar I, a history of prior antidepressant-induced mania, or rapid cycling (four or more mood episodes a year) are at the highest risk. If you’ve had one switch before, your chance of another jumps 3.2 times. And if you’re already showing mixed features-like irritability, racing thoughts, or impulsivity during a depressive episode-antidepressants can make things explode.
Which Antidepressants Are Riskiest?
Not all antidepressants are created equal. Tricyclics like amitriptyline and nortriptyline carry the highest risk-up to 25% chance of triggering mania. SNRIs like venlafaxine aren’t much better. SSRIs like sertraline or fluoxetine are safer, but still risky: around 8-10% switch rate. Even bupropion, often thought to be “mood-stabilizing,” can cause mania in vulnerable people.
Here’s the hard truth: the difference in risk between classes is small compared to the overall danger. The real issue isn’t which drug you pick-it’s whether you should be using any antidepressant at all.
The number needed to treat (NNT) for antidepressants in bipolar depression is 29.4. That means you’d need to treat nearly 30 people to help just one person feel better. Meanwhile, the number needed to harm (NNH) for a mood switch is about 200. At first glance, that sounds reassuring. But here’s the catch: 200 people is a lot. And when you’re dealing with someone already in crisis, even a 1 in 200 chance of triggering mania is too high-especially when safer, more effective options exist.
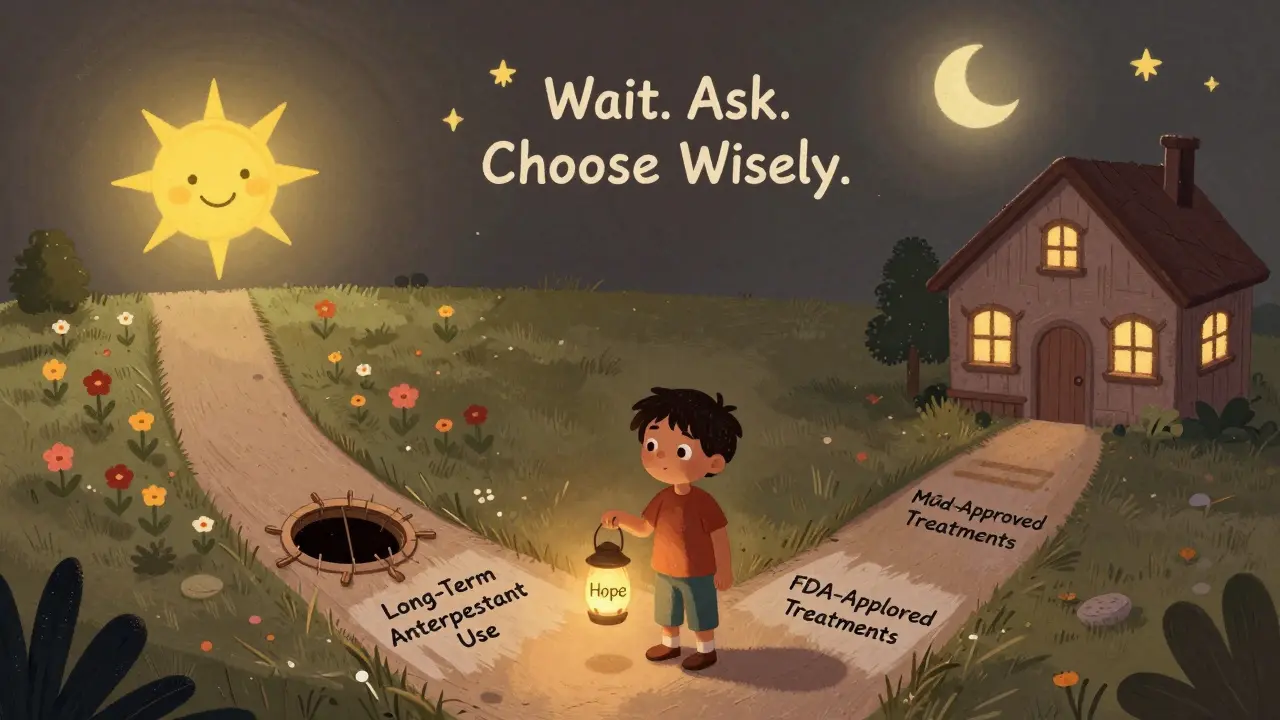
What Are the Alternatives?
The FDA has approved four medications specifically for bipolar depression-not one of them is a traditional antidepressant.
- Quetiapine (Seroquel): Works for about 50-60% of patients with less than 5% risk of switching.
- Lurasidone (Latuda): 50% response rate, only 2.5% switch risk.
- Cariprazine (Vraylar): 48% response rate, 4.5% switch risk.
- Olanzapine-fluoxetine combo (Symbyax): The only one that includes an SSRI, but it’s paired with an antipsychotic-and even then, switch risk is still lower than antidepressant monotherapy.
These drugs don’t just treat depression-they help stabilize mood long-term. They’re not fast-acting. It can take 4-6 weeks to see results. But they don’t risk sending you into a hospital.
Compare that to antidepressants: they often work faster-2-4 weeks. But that speed comes at a cost. Many people feel better for a few weeks, then crash into mania. And once that happens, recovery takes longer, and the risk of future episodes increases.

Why Do Doctors Still Prescribe Them?
Despite the guidelines, antidepressants are still prescribed to 50-80% of bipolar patients. In community clinics, it’s closer to 80%. In academic centers, it’s 50%. Why the gap?
One reason: misdiagnosis. About 40% of people with bipolar disorder are initially diagnosed with unipolar depression. They’re put on antidepressants-and never re-evaluated. Another reason: patient pressure. People in deep depression beg for something that works fast. Doctors, under time constraints, give them what they ask for.
There’s also inertia. Antidepressants are familiar. They’re cheap. They’re on every formulary. Mood stabilizers and atypical antipsychotics? They’re more expensive, come with their own side effects-weight gain, sedation, tremors-and require more monitoring.
But here’s the problem: when you treat bipolar depression with antidepressants alone, you’re not treating the illness. You’re treating a symptom-and ignoring the core instability.
When Might Antidepressants Be Okay?
Some experts argue they can be used safely-in very specific cases. Dr. Roger McIntyre, a leading bipolar researcher, says SSRIs or bupropion, when paired with a mood stabilizer and used short-term, may help certain patients. But he’s clear: only in Bipolar II, with no history of mania from antidepressants, no rapid cycling, and no mixed features.
The International Society for Bipolar Disorders (ISBD) agrees. Their 2022 guidelines say antidepressants should only be considered if:
- The depression is severe and hasn’t responded to two FDA-approved treatments
- There are no mixed features or rapid cycling
- It’s used as an add-on to a mood stabilizer or antipsychotic-not alone
- It’s stopped within 8-12 weeks, even if it’s working
At Tufts Medical Center, where Dr. Nassir Ghaemi leads the Mood Disorder Program, antidepressants are used in only 19% of bipolar cases. Most of those are brief, targeted, and closely watched.
What Happens If You Don’t Stop Them?
Long-term antidepressant use in bipolar disorder doesn’t just risk mania-it can change the course of the illness.
Studies show people who take antidepressants for more than 24 weeks are 37% more likely to have another depressive or manic episode. That’s not a coincidence. Antidepressants may interfere with the brain’s natural rhythm. They can promote rapid cycling, where mood swings become more frequent and harder to control.
One 2006 study found a 2.1 times higher chance of rapid cycling in patients on long-term antidepressants. Another found a 1.7-fold increase in overall episode frequency. These aren’t small effects. They’re life-altering.
And here’s the cruel twist: the more episodes you have, the harder it is to treat. Each switch makes the next one more likely. Antidepressants can literally make bipolar disorder worse over time.
What Should You Do If You’re on Antidepressants?
If you have bipolar disorder and are taking an antidepressant, ask yourself these questions:
- Was I diagnosed with bipolar disorder before starting this medication-or was I told I had “depression”?
- Have I ever had a period of high energy, reduced sleep, impulsivity, or racing thoughts while on this drug?
- Am I taking it alone-or with a mood stabilizer like lithium, valproate, or lamotrigine?
- How long have I been on it? More than 12 weeks?
If you answered yes to any of these, talk to your doctor. Don’t stop cold turkey. Withdrawal can cause rebound depression. But do ask: Is this still necessary? Are there safer options?
Bring your records. Ask for a full mood history review. Request screening for mixed features. Push for a discussion about FDA-approved alternatives. You have the right to know the risks-and the alternatives.
The Bigger Picture
Antidepressants for bipolar depression is a classic case of medical inertia. We keep doing what we’ve always done-even when the evidence says it’s harmful.
Pharmaceutical companies still market antidepressants aggressively for bipolar depression, even though the FDA hasn’t approved them for that use. Insurance companies often cover them easily, but not newer, more expensive mood stabilizers. And patients? They just want to feel better.
But feeling better in the short term can cost you years of stability. The goal isn’t just to lift mood-it’s to protect your life. And that means choosing treatments that don’t just treat depression, but prevent the next crash.
There’s hope on the horizon. New treatments like esketamine nasal spray show 52% response rates in bipolar depression with only 3.1% switch risk. Researchers are exploring genetic markers that might predict who’s most likely to switch. But until those become standard, the safest choice remains clear: avoid antidepressants unless absolutely necessary-and never alone.
Can antidepressants cause mania in bipolar disorder?
Yes. Antidepressants can trigger mania or hypomania in people with bipolar disorder, especially if used without a mood stabilizer. Studies show a 12% risk of switching in controlled trials, and up to 31% in real-world settings. The risk is highest with tricyclics and SNRIs, and in people with Bipolar I, rapid cycling, or prior antidepressant-induced mania.
Are SSRIs safer than other antidepressants for bipolar depression?
SSRIs carry a lower risk of mood switching-around 8-10%-compared to tricyclics (15-25%) or SNRIs. But they’re still not safe as monotherapy. Even SSRIs can trigger mania, especially in people with mixed features or a history of rapid cycling. They should only be used short-term and always paired with a mood stabilizer.
What are the FDA-approved treatments for bipolar depression?
The FDA has approved four medications specifically for bipolar depression: quetiapine (Seroquel), lurasidone (Latuda), cariprazine (Vraylar), and the combination of olanzapine and fluoxetine (Symbyax). These have proven efficacy with significantly lower risk of triggering mania than antidepressants alone.
How long should antidepressants be used in bipolar disorder?
According to the International Society for Bipolar Disorders (ISBD), antidepressants should be used for no longer than 8-12 weeks-even if they’re working. Longer use increases the risk of rapid cycling, episode recurrence, and treatment resistance. After that, they should be tapered off under medical supervision.
Can antidepressants make bipolar disorder worse over time?
Yes. Long-term antidepressant use (over 24 weeks) is linked to a 37% higher risk of recurrent depressive or manic episodes. They may disrupt the brain’s natural mood regulation, promote rapid cycling, and reduce the effectiveness of mood stabilizers. For many, they turn a manageable condition into a more volatile one.
Why do so many doctors still prescribe antidepressants for bipolar disorder?
Many doctors misdiagnose bipolar depression as unipolar depression-about 40% of cases are initially wrong. Others prescribe them because patients demand quick relief, or because antidepressants are cheaper and easier to access than FDA-approved alternatives. Community clinics prescribe them in 80% of cases, while academic centers follow guidelines more closely. Clinical inertia and lack of access to specialists keep outdated practices alive.


so i took sertraline for 8 months thinking i had 'depression'... turned out i was bipolar and i went full moon mode. like, i bought a kayak on credit and tried to paddle to canada. my mom had to ground me. thanks, big pharma. 🤡
antidepressants are for weak people who can't handle life. just get a job and stop whining. this is why america is falling apart.
While the data presented is compelling, I must emphasize the critical importance of differential diagnosis in mood disorders. The conflation of unipolar and bipolar depression remains a pervasive clinical challenge, particularly in primary care settings where psychiatric training is limited. The 12% switch rate in controlled trials is statistically significant, yet the real-world figures suggest systemic underdiagnosis rather than pharmacological malpractice alone.
Moreover, the comparison between NNT and NNH requires contextualization: while the number needed to harm appears favorable, the qualitative impact of a manic episode-including job loss, relational collapse, and legal consequences-far exceeds the statistical metrics. This is not merely a pharmacological issue, but a sociocultural one rooted in diagnostic inertia and access disparities.
The FDA-approved alternatives, while safer, carry their own burdens: weight gain, metabolic syndrome, and extrapyramidal symptoms. These are not trivial trade-offs, especially for patients with comorbid conditions. A one-size-fits-all approach is as dangerous as the overprescription it seeks to correct.
What we need is not demonization of antidepressants, but better tools for longitudinal mood tracking, accessible psychoeducation, and integrated care models that prioritize patient autonomy within a framework of evidence-based caution.
Let’s be real-antidepressants aren’t the villain here. The villain is the system that lets a 10-minute consult decide your brain’s fate. I’ve seen people get prescribed SSRIs like they’re Advil. No history. No follow-up. No clue they’re bipolar until they’re in the ER yelling at the ceiling fan. And then? They get blamed for ‘not taking meds right.’
Meanwhile, the real solution-long-term therapy, lithium monitoring, lifestyle work-isn’t covered by insurance unless you’re rich or have a PhD. We’re treating symptoms like they’re bugs to spray, not systems to understand.
And don’t get me started on how pharma pushes antidepressants like they’re the only game in town. They spend more on ads than on research for mood stabilizers. It’s not about what works. It’s about what sells.
People aren’t stupid. They just want to feel human again. If the system gave them real options instead of quick fixes, we wouldn’t be having this conversation.
OMG I KNEW IT. I told my therapist last year that antidepressants were dangerous for bipolar people and she said I was being dramatic. SHE’S A QUITTER. I had to go to a naturopath who gave me magnesium and told me to do breathwork. Now I’m stable. 🙌 The system is broken and they’re poisoning us. #AntidepressantsArePoison #WakeUpSheeple
the data is solid but nobody wants to hear it because meds are easier than therapy and therapy costs money and nobody wants to pay for it so they just keep popping pills like candy
I used to think healing was about fixing broken parts. Now I know it’s about learning to dance with the storm. Bipolar isn’t a defect-it’s a different frequency. Antidepressants try to mute the noise, but what if the noise is the signal? What if the mania isn’t the enemy, but the echo of a soul trying to break through a system that only values flatness?
I’ve been on lithium for 12 years. It’s not glamorous. I gain weight. I’m tired. I drink a lot of water. But I’ve never been hospitalized. I’ve held my kids through panic attacks. I’ve written poems in the dark that later became songs. The drugs didn’t save me. The stability did. And stability isn’t found in a pill bottle-it’s found in routines, in community, in saying no when the world screams yes.
We’ve turned mental health into a product. But healing isn’t purchased. It’s practiced. Every day. Even when you don’t feel like it. Even when the pills tell you to.
So yes, avoid antidepressants alone. But also-ask for the therapy you deserve. Demand the time your doctor should give you. Push for the labs, the tracking, the support. Because you’re not a diagnosis. You’re a human being trying to find your rhythm in a world that wants you silent.
Been on lamotrigine for 7 years. No mania. No crash. Just steady. I used to take fluoxetine-felt great for 3 weeks, then spent 3 days cleaning my apartment with a toothbrush and calling my ex at 3am. Not worth it. 🤦♂️
Also, if your doc won’t talk about alternatives, find a new doc. Seriously. Your brain isn’t a vending machine.
antidepressants are for weak minds. just meditate and be strong
so basically we’re all just lab rats for pharma’s profit and the doctors are too lazy to read the damn studies? 🙄 i’m starting a podcast called ‘My Psychiatrist is a Sales Rep’
My cousin’s son took antidepressants and now he’s in a mental hospital. That’s why we don’t trust doctors. They just want to sell pills. End of story.
the real conspiracy is that they want you dependent on meds so you dont ask why you're depressed in the first place. capitalism made you sad so they sell you pills to forget you're being exploited. also lithium is expensive so they don't want you to have it. check the stock prices of big pharma companies