Why Weight Gain Happens With Psychotropic Medications
Many people start taking psychotropic meds-like antidepressants, antipsychotics, or mood stabilizers-to feel better. But for a lot of them, something unexpected happens: they start gaining weight. Not a little. Sometimes 10 pounds, 20, even more. And it’s not just about clothes fitting tighter. This weight gain is tied to real health risks: higher blood sugar, bad cholesterol, high blood pressure, and a much shorter life expectancy.
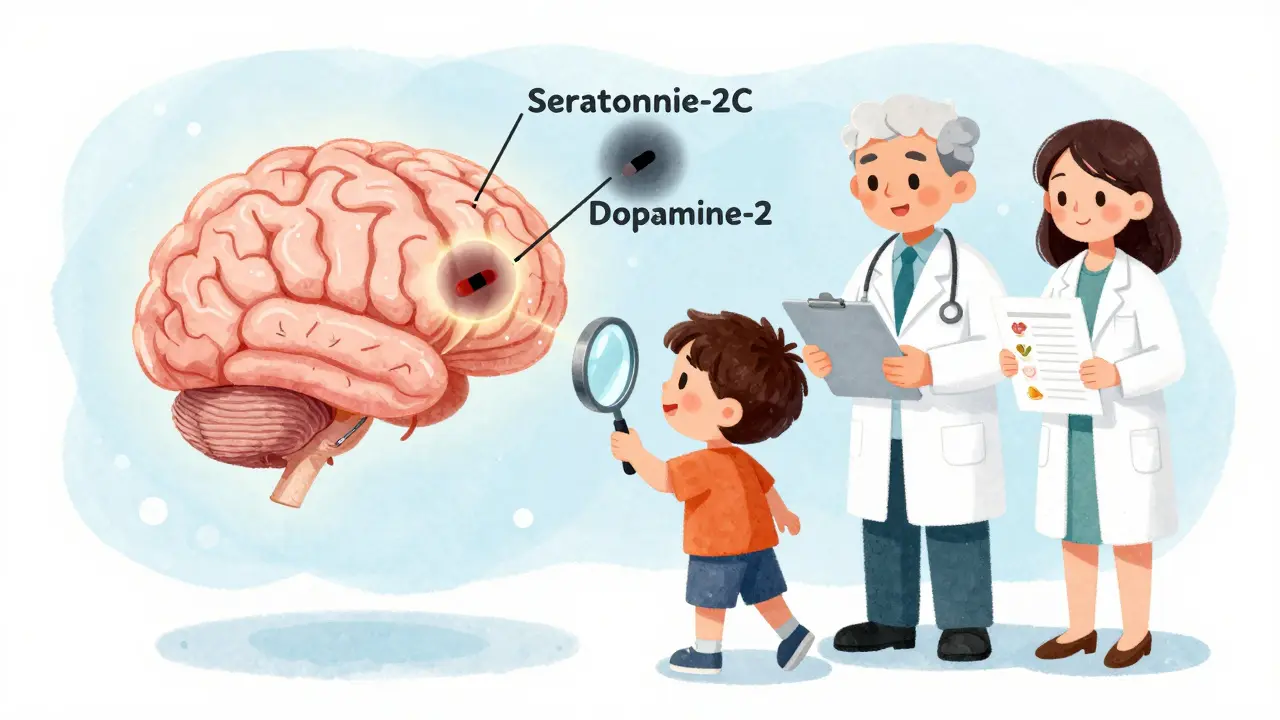
The science behind this isn’t new. Back in 1999, researchers found that second-generation antipsychotics (SGAs) were the biggest culprits. Today, we know why. These drugs block certain brain receptors-histamine-1, serotonin-2C, and dopamine-2-that normally help control appetite and how your body stores fat. When those signals get disrupted, hunger spikes, metabolism slows, and fat builds up, even if you’re eating the same as before.
Some medications are far worse than others. Olanzapine and clozapine? They can add 4 kilograms (almost 9 pounds) in just 10 weeks. By the end of the first year, some people gain 10 kilograms or more. In comparison, lurasidone causes less than 1 kilogram of gain, and paliperidone shows almost no change over a full year. It’s not a guess-it’s measurable, documented data from clinical trials and FDA labeling.
Which Medications Are Most Likely to Cause Weight Gain
If you’re on a psychotropic med and you’re seeing the scale creep up, it’s worth knowing which ones are most likely to cause this. Not all are created equal.
Among antipsychotics, the highest risk group includes:
- Clozapine and olanzapine - highest weight gain potential
- Quetiapine and risperidone - moderate risk
- Paliperidone and iloperidone - mild to moderate
- Aripiprazole, ziprasidone, asenapine, and lurasidone - lowest risk
For antidepressants, the big offenders are mirtazapine, amitriptyline, nortriptyline, paroxetine, and phenelzine. Even mood stabilizers like lithium and valproate can add pounds over time.
Here’s what matters: if you’re on olanzapine and gaining weight fast, switching to aripiprazole or lurasidone could cut your risk in half. But it’s not a simple swap. Stopping or changing meds can trigger relapse. That’s why decisions like this need to be made with your doctor-not on your own.
How Weight Gain Affects Your Long-Term Health
Weight gain from these meds isn’t just a body image issue. It’s a life expectancy issue. People with serious mental illnesses already live 10 to 20 years less than the general population. A big part of that gap comes from metabolic problems caused by the very drugs meant to help them.
Weight gain often leads to insulin resistance, which turns into type 2 diabetes. It raises triglycerides and lowers good cholesterol. It increases blood pressure. Together, these form metabolic syndrome-a cluster of conditions that double your risk of heart disease and stroke.
Studies show that 30% to 50% of people on high-risk antipsychotics gain enough weight to meet obesity criteria. That’s 2 to 3 times the rate seen in the general population. And here’s the kicker: once you’re on these meds, losing weight gets harder. One study found that people on psychotropics lost 1.6% less weight over a year than those not on them-even when both groups followed the same diet and exercise plan.
This isn’t about willpower. It’s biology. Your body is fighting against you because of how the medication changes your hunger signals and energy use.
Proven Ways to Fight Weight Gain
There are three main ways to handle this: switch meds, add a helper drug, or change your lifestyle. All three work-but not equally, and not for everyone.
Switching medications is the most direct approach. If you’re on olanzapine and gaining 10 pounds a month, switching to aripiprazole or lurasidone might stop the gain entirely. But don’t rush this. Your psychiatrist needs to monitor you closely. Switching too fast can cause anxiety, psychosis, or depression to come back.
Adding metformin is one of the most studied and effective options. Metformin, a diabetes drug, helps your body use insulin better. In multiple trials, people who took metformin along with their antipsychotic lost 2 to 4 kilograms more than those who didn’t. It’s safe, cheap, and widely available. Some doctors now prescribe it upfront for people starting high-risk meds.
Topiramate, an older seizure and migraine drug, also helps. Studies show it can reduce weight by 3 to 5 kilograms over several months. But it can cause brain fog, tingling, or memory issues-so it’s not for everyone.
And then there’s GLP-1 agonists like semaglutide. Originally for diabetes, they’re now being tested for psychiatric patients. Early results show 5% to 8% weight loss. These are newer, more expensive, and not yet approved for this use-but they’re coming.
Lifestyle Changes That Actually Work
Just telling someone to “eat better and exercise” doesn’t cut it when their medication is hijacking their appetite and energy. But structured programs do.
Successful plans include:
- Weekly sessions with a dietitian who understands psychiatric meds
- Meal plans that account for increased hunger-like adding protein and fiber to stay full longer
- Exercise routines tailored to fatigue or low motivation-starting with 10-minute walks, three times a week
- Behavioral therapy to manage emotional eating triggered by anxiety or depression
One study showed that patients in a multidisciplinary program (psychiatrist + dietitian + exercise coach) lost 3 times more weight than those getting standard care. The key? Consistency. Not perfection.
Apps like Moodivator, approved by the FDA in 2021, help track food, mood, and activity. In a 2022 trial, users lost 3.2% more weight than those without the app. It’s not magic-but it’s a tool that works when used daily.

What to Ask Your Doctor
If you’re on psychotropic medication and worried about weight, here’s what to say:
- “What’s the weight gain risk with this medication compared to others?”
- “Can we start metformin now to prevent weight gain?”
- “Can I get a referral to a dietitian who works with psychiatric patients?”
- “Are there lower-risk alternatives that still work for my symptoms?”
- “Can we check my blood sugar, cholesterol, and waist size every 3 months?”
Don’t wait until you’ve gained 15 pounds. Ask early. Get baseline numbers before you start. Track your waist circumference-it’s a better early warning sign than the scale.
Also, know this: you’re not alone. About 1 in 5 people stop their meds because of weight gain. That’s dangerous. The goal isn’t to avoid meds-it’s to manage the side effects so you can stay on them safely.
What’s Changing in 2026
The field is moving fast. The FDA now requires drug labels to include specific weight gain risk levels. Hospitals like the VA have made quarterly metabolic checks mandatory for all patients on antipsychotics-and their early detection rates jumped 15%.
Research is now looking at genetics. Some people have a variation in the MC4R gene that makes them far more likely to gain weight on certain meds. In the next few years, we may see genetic tests used to pick the safest drug for each person.
Big health organizations are finally working together. The American Psychiatric Association and the American Diabetes Association now have joint guidelines for treating diabetes in people with mental illness. That’s huge. It means weight management isn’t an afterthought-it’s part of psychiatric care.
Final Thoughts: You Can Have Both Stability and Health
Managing weight while on psychotropic meds isn’t about choosing between mental health and physical health. It’s about getting both. You don’t have to accept weight gain as inevitable. You don’t have to quit your meds. You don’t have to suffer in silence.
With the right plan-medication choice, metformin, diet, movement, and regular check-ins-you can stabilize your mood and protect your body. It takes teamwork. It takes time. But it’s possible. And it’s worth it-for your energy, your confidence, and your future.

