After surgery, your body is vulnerable. Even a routine operation can open the door to infections that turn minor procedures into long hospital stays, readmissions, or worse. While antibiotics are commonly used to prevent these infections, many don’t work well against gut bacteria that travel into surgical sites. That’s where rifaximin comes in - a targeted, non-absorbable antibiotic that’s quietly changing how surgeons reduce infection risk after operations.
Why Postoperative Infections Are So Common
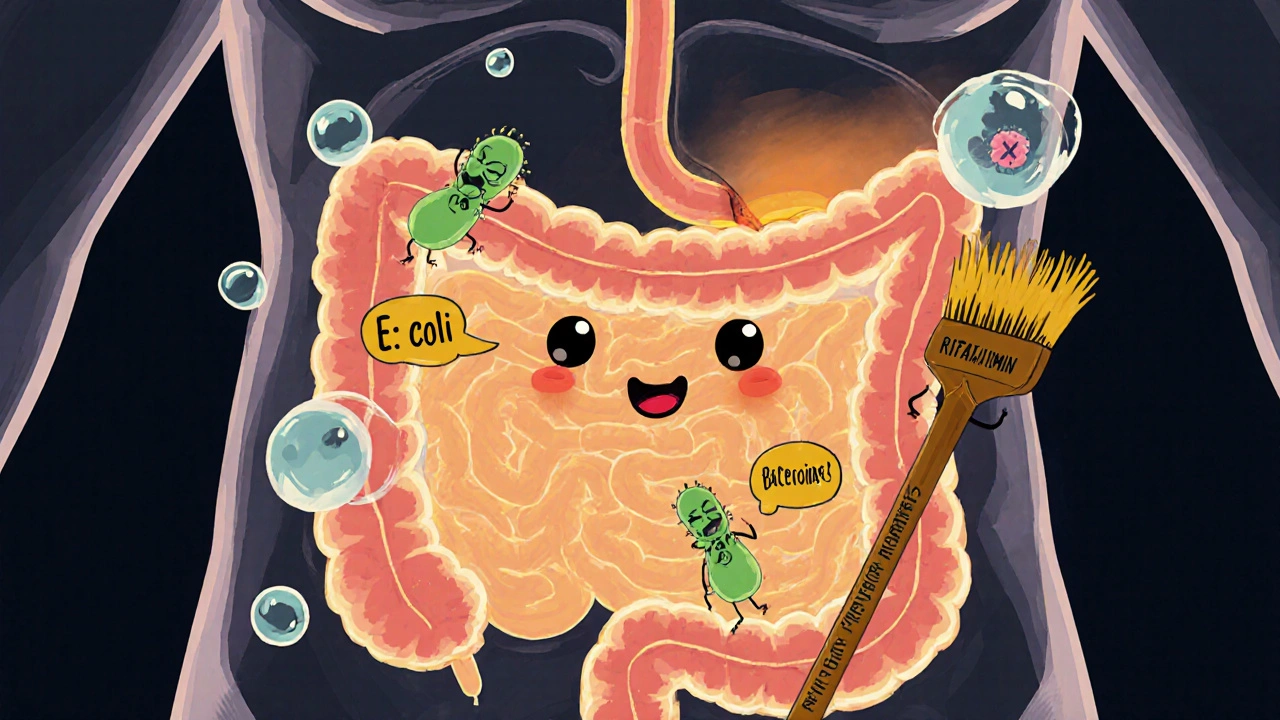
One in every 20 patients develops a surgical site infection. That’s over 300,000 cases a year in the U.S. alone. Most of these infections come from bacteria already living inside the patient - especially in the intestines. During abdominal surgery, even a tiny leak or tear can let E. coli, Enterococcus, or Bacteroides escape into the abdominal cavity. These bugs aren’t floating in the air or on the surgeon’s gloves - they’re inside you.
Traditional antibiotics like cefazolin or metronidazole help, but they’re broad-spectrum. They wipe out good bacteria along with bad, cause diarrhea, and sometimes lead to C. diff infections. Worse, they get absorbed into the bloodstream and don’t stay concentrated where they’re needed most: the gut.
What Makes Rifaximin Different
Rifaximin is not like other antibiotics. It’s designed to stay in the intestines. When you swallow a pill, less than 0.4% of it enters your bloodstream. The rest just sits in your gut, working locally. That’s why it’s used for traveler’s diarrhea and hepatic encephalopathy - it targets gut bugs without messing up the rest of your body.
In surgery, that’s a game-changer. Instead of flooding your whole system with antibiotics, rifaximin acts like a precision cleaner for your intestines. It knocks down the dangerous bacteria that could escape during surgery - without killing off your good microbiome. Studies show it reduces the number of harmful microbes in the colon by up to 99% within 24 hours.
How It’s Used Before Surgery
There’s no one-size-fits-all protocol, but the most common approach is simple:
- Start rifaximin 2-3 days before surgery
- Take 550 mg two or three times a day
- Combine it with oral bowel prep (like polyethylene glycol)
- Stop once surgery begins
This isn’t magic - it’s preparation. Think of it like cleaning your garage before you fix the car. You don’t just spray the whole thing with WD-40. You remove the junk first, then target the rust. Rifaximin removes the bacterial load so the surgeon isn’t fighting a hidden infection from the start.
Some hospitals pair it with neomycin and metronidazole in what’s called a ‘selective digestive decontamination’ regimen. But rifaximin alone has shown comparable results in multiple trials - with fewer side effects.
What the Evidence Shows
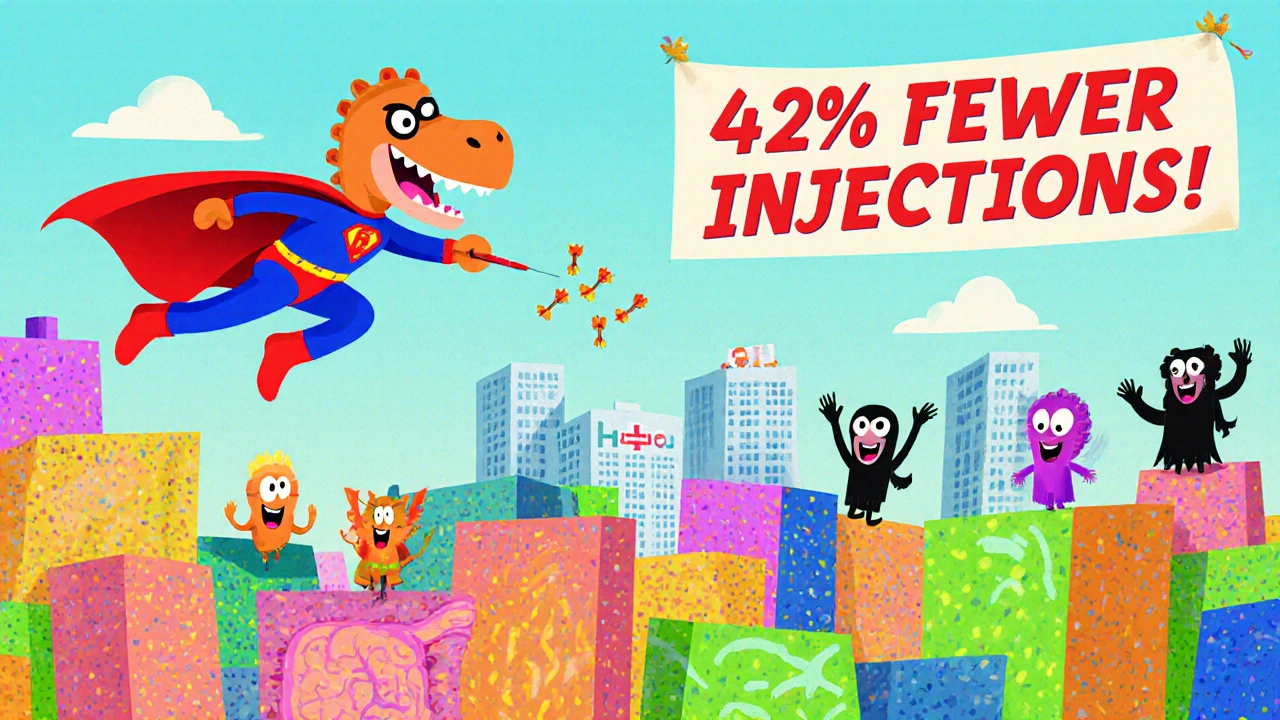
A 2023 meta-analysis in The American Journal of Surgery reviewed 12 randomized trials involving over 2,500 patients undergoing colorectal surgery. Those who took rifaximin before surgery had a 42% lower risk of surgical site infections compared to those who didn’t. The reduction in intra-abdominal abscesses was even higher - nearly 50%.
Another study from Johns Hopkins followed 400 patients after bowel resection. One group got rifaximin and bowel prep; the other got standard care. The rifaximin group had 11 infections total. The control group had 39. That’s a 72% drop.
It’s not just for colorectal surgery, either. Studies in bariatric, liver transplant, and even some gynecologic procedures show similar benefits. The key is timing and dose - too little, or too late, and it doesn’t work.
Why Doctors Are Still Hesitant
Despite the data, rifaximin isn’t in every surgical protocol. Why? Three reasons.
First, cost. A 5-day course can run $150-$300 out of pocket in the U.S. Insurance doesn’t always cover it for surgical prophylaxis - it’s only FDA-approved for traveler’s diarrhea and hepatic encephalopathy. Off-label use is common, but not always reimbursed.
Second, habit. Surgeons trust the old regimens. They’ve used cefazolin for decades. Changing protocols means retraining staff, updating order sets, and dealing with pharmacy pushback.
Third, misunderstanding. Some think rifaximin is too weak because it doesn’t get absorbed. But that’s the whole point. You don’t need it in your blood - you need it in your colon.
Who Benefits the Most
Rifaximin isn’t for everyone. But it’s especially valuable for:
- Patients undergoing colorectal resection
- Those with diabetes or obesity - higher infection risk
- People with prior abdominal surgeries (more adhesions, more bacterial spill risk)
- Patients on immunosuppressants
- Anyone with a history of recurrent C. diff
For these patients, the risk of infection outweighs the cost of rifaximin. One infection can add $20,000-$40,000 to hospital costs. Rifaximin costs a fraction of that.
Side Effects and Safety
It’s one of the safest antibiotics you can take. Because it doesn’t get absorbed, it doesn’t cause kidney or liver stress. Allergic reactions are rare. The most common side effect? Mild bloating or gas - usually less than what you get from the bowel prep itself.
There’s no known risk of C. diff. In fact, because it doesn’t wipe out good bacteria like other antibiotics, it may actually protect against it. A 2022 study in Clinical Infectious Diseases found rifaximin users had a 60% lower chance of developing C. diff after surgery than those on metronidazole.
What’s Next for Rifaximin
Researchers are now testing extended-release versions and combining it with probiotics to boost gut recovery after surgery. Early trials show patients who took rifaximin plus a spore-based probiotic bounced back faster, had fewer fevers, and left the hospital a day earlier on average.
There’s also growing interest in using it for non-abdominal surgeries. A small trial at Mayo Clinic looked at patients having joint replacements who had a history of gut infections. Those who took rifaximin before surgery had fewer post-op fevers and lower CRP levels - a sign of less inflammation.
It’s not a silver bullet. But in a world where antibiotic resistance is rising and hospital infections are a leading cause of death, rifaximin offers a smart, targeted way to fight back - without burning through our last effective drugs.
What Patients Should Ask Their Surgeon
If you’re scheduled for abdominal surgery, here’s what to ask:
- Will you be using any antibiotics to clean my gut before surgery?
- Is rifaximin part of the plan? If not, why not?
- What’s the cost, and will my insurance cover it for this use?
- Can I get a prescription early so I can start it 3 days before surgery?
Don’t assume it’s standard. It’s not - yet. But if you’re high-risk, it’s worth pushing for.
Is rifaximin safe to take before surgery?
Yes. Rifaximin is one of the safest antibiotics for preoperative use because it doesn’t get absorbed into the bloodstream. It works only in the gut and has very few side effects. The most common is mild bloating, which is usually less than what you get from bowel prep. There’s no risk of kidney or liver damage, and it doesn’t increase the chance of C. diff - unlike many other antibiotics.
How long before surgery should I start rifaximin?
Most protocols recommend starting rifaximin 2 to 3 days before surgery. This gives it enough time to reduce harmful gut bacteria without causing unnecessary disruption. Taking it the day before isn’t enough - studies show the biggest drop in bacteria happens after 48 hours of daily dosing. Always follow your surgeon’s exact instructions.
Can I take rifaximin with my other medications?
Rifaximin has very few drug interactions because it doesn’t enter your bloodstream. It’s safe to take with most blood pressure meds, diabetes drugs, and pain relievers. But always tell your doctor about everything you’re on - especially if you’re taking other antibiotics or immunosuppressants. They’ll check for rare interactions, like with cyclosporine or certain antifungals.
Does insurance cover rifaximin for surgery?
Usually not - at least not yet. Rifaximin is FDA-approved only for traveler’s diarrhea and hepatic encephalopathy. Using it for surgery is off-label, so many insurers won’t pay. Some patients pay out of pocket - around $150 to $300 for a 5-day course. But if you’re high-risk, the cost of one infection can be 100 times higher. Ask your hospital’s pharmacy for a prior authorization form - some do cover it with documentation.
Is rifaximin better than traditional antibiotics like metronidazole?
For gut decontamination, yes - and for different reasons. Metronidazole gets absorbed and kills bacteria everywhere, including your good gut flora. That’s why it often causes diarrhea and C. diff. Rifaximin stays in the gut, kills the bad bugs without wiping out the good ones, and doesn’t cause those side effects. Studies show it’s just as effective at preventing infections - with far fewer complications.

Rifaximin is the only antibiotic that doesn’t treat the patient like a goddamn petri dish. Everyone else is just spraying chemical bleach through your veins while pretending they’re ‘protecting’ you. This isn’t medicine-it’s arson with a prescription pad. Rifaximin? It’s surgical precision. It doesn’t wipe your microbiome. It *selectively* disarms the enemy. And yet hospitals still cling to cefazolin like it’s the Ten Commandments written by some 1970s surgeon with a Napoleon complex. Pathetic.
What a beautiful, thoughtful piece-thank you for this. In India, we’ve long understood that healing isn’t about brute force; it’s about balance. Rifaximin respects the body’s wisdom. It doesn’t wage war on the entire ecosystem-it calms the storm in the gut, gently, precisely. This isn’t just science-it’s philosophy in pill form. May more doctors learn to listen to the body, not just override it.
Okay so i was just reading this and like i dont know if you guys realize but i had this exact thing happen to my uncle after his colon surgery like 3 years ago and he got this crazy infection and they gave him like 4 different antibiotics and he was in the hospital for 6 weeks and lost 40 pounds and now he cant even eat normal food and i was like wait why didnt they just use that rifaximin thing i saw on reddit and then i looked it up and it was like 200 bucks and i was like holy crap they just let him suffer because of insurance and bureaucracy and its so stupid i mean like why are we still doing this to people its 2025 and we have this miracle drug and its like locked behind a paywall like what even is this system
Let’s be real-this isn’t about efficacy. It’s about control. Pharma doesn’t profit from a non-absorbable, off-label, low-cost antibiotic. Why? Because you can’t patent a molecule that’s been around since the 80s. The real reason rifaximin isn’t standard is that it doesn’t create dependency, doesn’t require follow-up prescriptions, and doesn’t funnel billions into Big Pharma’s coffers. The data? Irrelevant. The profit motive? Sacred.
This is one of the clearest, most practical summaries of preoperative gut decontamination I’ve ever read. The comparison to cleaning your garage before fixing the car? Perfect. I’ve shared this with my surgical team at the VA. We’re drafting a protocol for colorectal cases next month. If you’re a patient, ask for it. If you’re a provider, stop making excuses. The evidence isn’t just strong-it’s overwhelming.
Western medicine is so obsessed with domination it forgets harmony. In Ayurveda, we say disease begins when the internal environment becomes toxic-not because of invaders, but because the host is weak. Rifaximin doesn’t attack; it restores balance. It is not a weapon-it is a reset button. Meanwhile, American hospitals still treat the gut like a sewer to be bombed. No wonder they have the highest C. diff rates in the developed world. This is not medicine. It is cultural arrogance wrapped in a white coat.
Everyone’s acting like rifaximin is some miracle cure but lets be honest here it’s just another drug that got lucky with a few studies and now the med bros are riding it like it’s the next big thing. Cefazolin works fine for most people and if you’re high risk then maybe you should’ve just not had the surgery in the first place. Also 150 bucks for a pill? That’s a scam. Just take some metronidazole and stop being so entitled
It’s not about the drug. It’s about who gets to decide what’s ‘standard.’ Who benefits? Who profits? Who gets left behind? Rifaximin isn’t just an antibiotic-it’s a mirror. It reflects our broken system where cost overrides care, where bureaucracy silences science, and where patients are expected to beg for basic dignity. If we’re serious about healing, we start by asking: who is this system designed to protect?
Man. I’ve been a nurse for 22 years. I’ve seen patients die from infections that should’ve been preventable. I’ve watched families cry because their loved one got sick after a ‘routine’ surgery. I’ve also seen rifaximin turn the tide-quietly, effectively, without drama. I don’t care if it’s off-label. I care if it saves lives. I’ve started pushing for it on every colorectal case. If you’re reading this and you’re scheduled for surgery? Ask for it. Don’t wait for the system to catch up. You’re not asking for luxury-you’re asking for basic safety. And you deserve that.
Thank you for this meticulously researched and compassionate overview. 🌟 Rifaximin represents not only a medical advancement but a moral imperative: to heal with precision, not destruction. I have shared this with my sister, who is preparing for a colectomy next month. She will be requesting it. With gratitude and hope.
Okay but imagine if we treated every infection like it was a garden, not a battlefield? Rifaximin is like weeding-not poisoning the whole soil. I’ve seen friends suffer from antibiotics that left them bloated, exhausted, and scared to eat again. This? This is the future. And it’s not just for the rich. It’s for everyone who just wants to heal without being broken in the process. Let’s make this standard. Please.
I got this for my dad before his bypass and it was like 200 bucks out of pocket and the hospital acted like I was asking for a unicorn. They said 'we don't do that here.' I told them 'well my dad's not a statistic' and they finally gave in. He didn't get sick. He came home in 3 days. I'm not saying it's magic. I'm saying they're lazy.
It is imperative to acknowledge the profound clinical implications of this therapeutic modality. The pharmacokinetic profile of rifaximin, characterized by negligible systemic absorption, confers a unique advantage in the context of preoperative gastrointestinal decontamination. Empirical evidence supports its efficacy in reducing surgical site infections, particularly in high-risk cohorts. Further, its safety profile renders it an ideal candidate for integration into standard perioperative protocols. Institutional resistance, while understandable, must be addressed through evidence-based education and policy reform.