When your big toe suddenly swells up, turns red, and feels like it’s on fire-even the weight of a bedsheet becomes unbearable-you’re not just having a bad night. You’re having a gout attack. This isn’t just "bad arthritis." It’s a specific, painful reaction caused by crystals forming in your joints, and it’s tied directly to how your body handles uric acid. Many people think gout is just about eating too much steak or drinking too much beer. But the real story is deeper, more complex, and far more treatable than most realize.
What Exactly Is Uric Acid, and Why Does It Cause Pain?
Uric acid is a waste product your body makes when it breaks down purines-natural substances found in your cells and in certain foods. Most people’s bodies handle this just fine. But in gout, something goes wrong. Your blood ends up with too much uric acid, and when it hits 6.8 mg/dL or higher, it starts to form sharp, needle-like crystals in your joints. These crystals don’t just sit there quietly. They trigger your immune system like an alarm.
Your body sees these crystals as invaders. Macrophages-your immune cells-swarm the area and activate something called the NLRP3 inflammasome. That sets off a chain reaction, releasing interleukin-1β, a powerful inflammatory signal. That’s what causes the swelling, heat, and intense pain. It’s not the uric acid itself hurting you. It’s your body’s overreaction to the crystals.
Here’s the twist: humans are one of the only mammals that can’t break down uric acid fully. Most animals have an enzyme called uricase that turns it into something harmless. We lost that gene millions of years ago. That’s why gout is so common in people but rare in dogs or cats.
Why Do Some People Have High Uric Acid and Others Don’t?
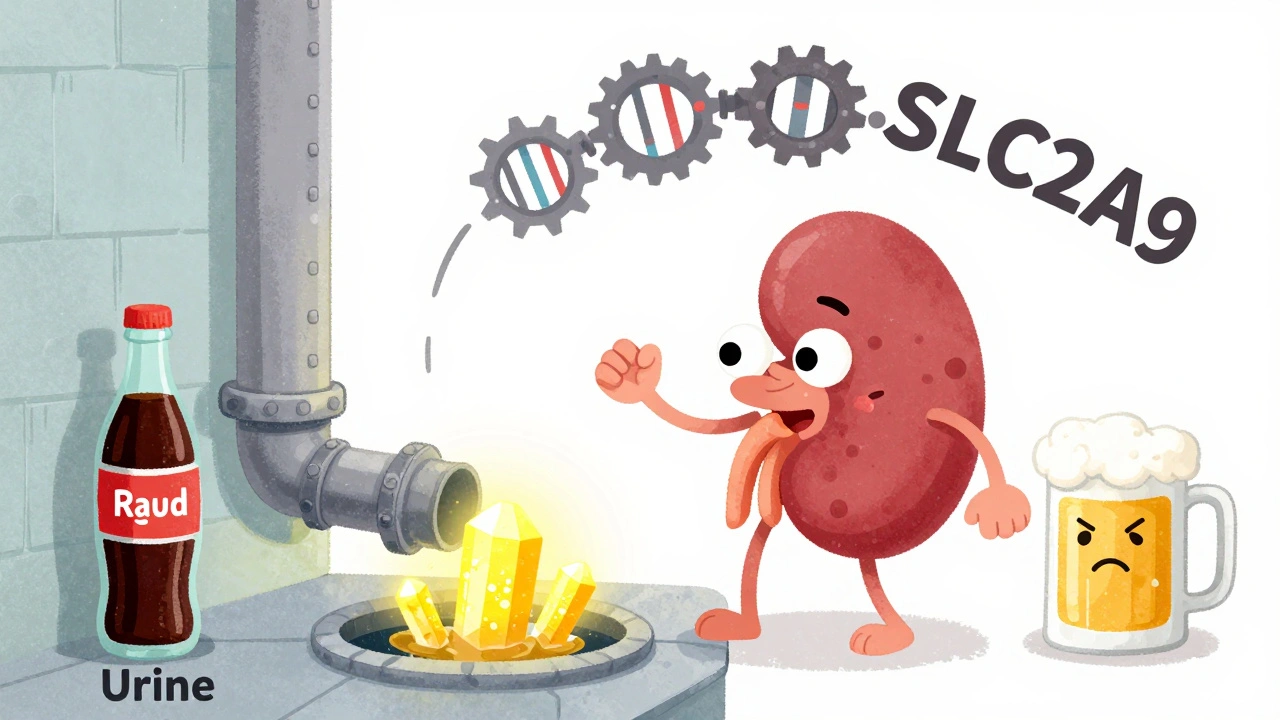
About 90% of gout cases come from your kidneys not flushing out enough uric acid. The other 10% are from your body making too much. Genetics play a huge role-up to 60% of your uric acid levels are determined by your DNA. Genes like SLC2A9, SLC22A12, and ABCG2 control how your kidneys reabsorb or dump uric acid. If these genes don’t work right, your body holds onto too much.
It’s not just genetics, though. Certain medications can make it worse. Thiazide diuretics (often used for high blood pressure) increase gout risk by 30-50%. Even low-dose aspirin (75-325 mg daily) can interfere with uric acid removal. Chronic alcohol use, especially beer, does too. Beer isn’t just alcohol-it’s packed with purines. A single 12-ounce serving can raise your risk by nearly 50%.
And then there’s fructose. Sugary drinks, sodas, fruit juices-anything with high-fructose corn syrup-spikes uric acid by 20-30%. That’s because fructose breaks down in your liver and depletes ATP, which then turns into purines, which turn into uric acid. It’s a hidden trigger most people never connect to their pain.
What Triggers a Gout Attack? It’s Not Just Food
Many think a gout attack happens because you ate a steak or drank a six-pack. But attacks usually come from sudden changes-not just the food itself. Here’s what really sets them off:
- Rapid changes in uric acid levels: Whether your level shoots up or drops fast, it can shake loose crystals and trigger inflammation. That’s why starting a uric acid-lowering drug like allopurinol can cause a flare in the first few months.
- Dehydration: When you’re not drinking enough water, your urine output drops below 1.5 liters a day. That means less uric acid gets flushed out, and concentration builds up in your joints.
- Joint injury: Even a minor bump or twist can dislodge crystals in a joint that’s already overloaded.
- Medical or surgical stress: Illness, surgery, or even intense physical exertion can trigger an attack.
- Stopping medication: If you stop your urate-lowering drug, your uric acid rebounds in just 2-4 weeks-and so do the attacks.
And here’s something most people don’t know: lowering uric acid too fast during a flare won’t help. In fact, it can make it worse. That’s why you can’t just pop a pill when the pain hits and expect it to vanish. The treatment has to be planned.
How Are Gout Attacks Treated When They Happen?
When you’re in the middle of an attack, your goal is to stop the inflammation fast. There are three main options, and your doctor will pick based on your health history:
- NSAIDs: Indomethacin (50 mg three times a day) is common. Ibuprofen or naproxen work too. But if you have kidney problems, stomach ulcers, or heart issues, these aren’t safe.
- Colchicine: Taken at 0.6 mg three times a day for 4-7 days. It’s effective but can cause diarrhea in 10-20% of people. Lower doses (0.6 mg once or twice daily) are now used for prevention, not just acute treatment.
- Corticosteroids: Prednisone (30-40 mg daily for 5 days, then tapered) is great if you can’t take NSAIDs or colchicine. It can be taken orally or injected directly into the joint.
These don’t fix the root problem. They just calm the fire. If you stop after the pain goes away, the crystals are still there. And they’ll come back.
Long-Term Strategy: Lowering Uric Acid for Life
This is where most people fail. They treat the flare and think they’re done. But gout isn’t cured by pain relief. It’s managed by keeping your blood uric acid below 6 mg/dL-ideally 5 mg/dL if you have tophi (those visible lumps under the skin).
The first-line drug is allopurinol. You start at 100 mg a day and increase by 100 mg every few weeks until you hit your target. Most people need 300-600 mg daily. Some need up to 800 mg. It’s safe for most, but rare cases can cause a serious skin reaction called allopurinol hypersensitivity syndrome (less than 0.4% of users).
If allopurinol doesn’t work or causes a reaction, febuxostat (40-80 mg daily) is the next option. It works differently-it blocks uric acid production instead of helping your kidneys flush it out.
For people with healthy kidneys, probenecid (250-2000 mg daily) helps the kidneys excrete more uric acid. But if your kidney function is below 50 mL/min, it won’t work well.
Here’s the critical part: you need to take these drugs every day, even when you feel fine. And you must start them with anti-inflammatory protection. For the first 6 months, take low-dose colchicine (0.6 mg once or twice daily). Studies show this cuts flare risk by 50-75%. Skipping this step is like lighting a match next to gasoline.
Diet and Lifestyle: What Actually Helps?
Diet matters-but not how you think. You don’t need to go vegan or cut out all meat. You need to be smart about it.
- Avoid: Organ meats (liver, kidney), shellfish (shrimp, mussels), and sugary drinks. These are the big three triggers.
- Limit: Beer and spirits. Wine has less impact, but still not risk-free.
- Do more of: Low-fat dairy. One to two servings a day lowers your risk by 43%. Cherries? Some evidence they help. Water? Drink at least 2 liters a day. It’s the cheapest, most effective treatment.
And yes, weight loss helps-if you’re overweight. Losing even 10 pounds can lower uric acid by 1-2 mg/dL. But crash diets or fasting? Those can trigger flares. Slow, steady change is the only way.

What Happens If You Don’t Treat It?
Left unchecked, gout isn’t just painful-it’s destructive. Repeated attacks lead to joint damage, bone erosion, and tophi. These are hard lumps of uric acid crystals that form under the skin, often on fingers, elbows, or ears. They can break through the skin and become infected.
But here’s the good news: if you keep your uric acid below 5 mg/dL for a full year, 70% of people with tophi see them completely disappear. That’s not a guess. That’s from the 2023 American College of Rheumatology meeting. It’s reversible.
And it’s not just your joints. High uric acid is linked to kidney disease, high blood pressure, and heart problems. Treating gout isn’t just about walking without pain. It’s about protecting your whole body.
What’s Next? New Treatments on the Horizon
Researchers are now targeting the inflammation at its source. Drugs like dapansutrile, which block the NLRP3 inflammasome, have shown in trials that they can cut flare duration by 40% compared to placebo. These aren’t available yet, but they’re the first treatments designed to stop the immune response itself-not just the uric acid.
Another area of interest? The gut microbiome. Early studies suggest certain probiotics might help your body break down purines more efficiently, lowering uric acid by 10-15%. It’s still experimental, but it opens up a whole new way to think about gout management.
Final Thoughts: Gout Is Manageable, But Not Optional
You can’t ignore gout. It doesn’t go away on its own. You can’t treat it with painkillers alone. And you can’t stop your medication when you feel better. This is a lifelong condition that requires daily attention.
The key is simple: know your uric acid level. Take your meds every day. Drink water. Avoid beer and sugary drinks. Eat more low-fat dairy. And work with your doctor to get your number below 6 mg/dL-and keep it there.
If you do, you won’t just avoid another attack. You’ll stop the damage before it starts. And you’ll get your life back-not just your big toe.


Been dealing with gout for 5 years now and honestly the water tip saved me 🥵 I used to drink soda like it was water now i chug 3L a day and my flares are way less intense. Also low fat milk is magic. No joke. My doc was skeptical but i tried it and boom no more weekly pain.
So just don’t eat shrimp and drink beer. Done.
The oversimplification here is almost offensive. Yes, diet plays a role-but the real issue is the evolutionary loss of uricase, which makes humans uniquely vulnerable. Most people don’t realize that even with perfect diet, if your SLC2A9 variant is dysfunctional, you’re genetically primed for hyperuricemia. This is not a lifestyle failure-it’s a biochemical inevitability for many. The fact that pharmaceutical companies push allopurinol as the first-line fix without genetic screening is a systemic failure. We’re treating symptoms while ignoring the genomic architecture of the disease. And don’t get me started on how fructose metabolism bypasses normal purine regulation via ATP depletion. This isn’t just about soda-it’s about how modern biochemistry has outpaced human adaptation. The NLRP3 inflammasome isn’t some abstract concept-it’s the literal ignition switch for your immune system’s overreaction. If you’re not targeting that, you’re just rearranging deck chairs on the Titanic.
I know how scary it is to get your first gout attack-it feels like your body is betraying you. But please don’t give up. I was diagnosed 3 years ago and thought I’d never eat anything fun again. Turns out, it’s not about restriction, it’s about rhythm. I take my allopurinol every night like brushing my teeth. I drink water before coffee. I swap soda for sparkling water with lime. And I eat yogurt every morning. It’s not perfect, but it’s sustainable. The pain fades. The tophi shrink. You get your life back. You’re not broken-you’re just learning a new way to care for yourself. And that’s okay.
ALLOPURINOL IS A TOXIN!!! THEY’RE HIDING THE TRUTH!! The FDA knew about the hypersensitivity syndrome since the 80s!! And why do you think they push it? Because Big Pharma owns the journals!! And don’t tell me about “low-dose colchicine” - that’s just another poison to mask the symptoms!! The REAL cause is glyphosate in our food!! It messes with your liver enzymes!! I’ve been detoxing with activated charcoal and apple cider vinegar for 14 months-my uric acid dropped 3.2 points!! No pills!! No drugs!! Just nature!! You’re being manipulated!!
i had a gout flare last month and i just took ibuprofen and it went away so i stopped taking the pills. why do i need to take them forever? i dont feel sick. also i like beer and i dont want to quit. its just a toe thing right? why are doctors so dramatic? i think they just want to sell more medicine.
I read this whole thing twice. I didn’t know gout was this complex. I thought it was just about what you ate. Now I understand why my dad had to change so much. I’m going to talk to him tonight. Maybe he’ll let me help him track his water intake. He’s stubborn but I think he’ll listen.
Just wanted to say thank you for writing this with so much clarity. I’ve been managing gout for over a decade and I’ve never seen someone explain the NLRP3 inflammasome and uricase evolution in a way that made sense to someone without a medical degree. The part about rapid changes triggering flares-even when lowering uric acid-is something my rheumatologist mentioned once, but I forgot. I’m starting low-dose colchicine tomorrow as a preventive, and I’m actually not scared anymore. This isn’t just a medical article. It’s a lifeline. I’ll be sharing it with my support group.