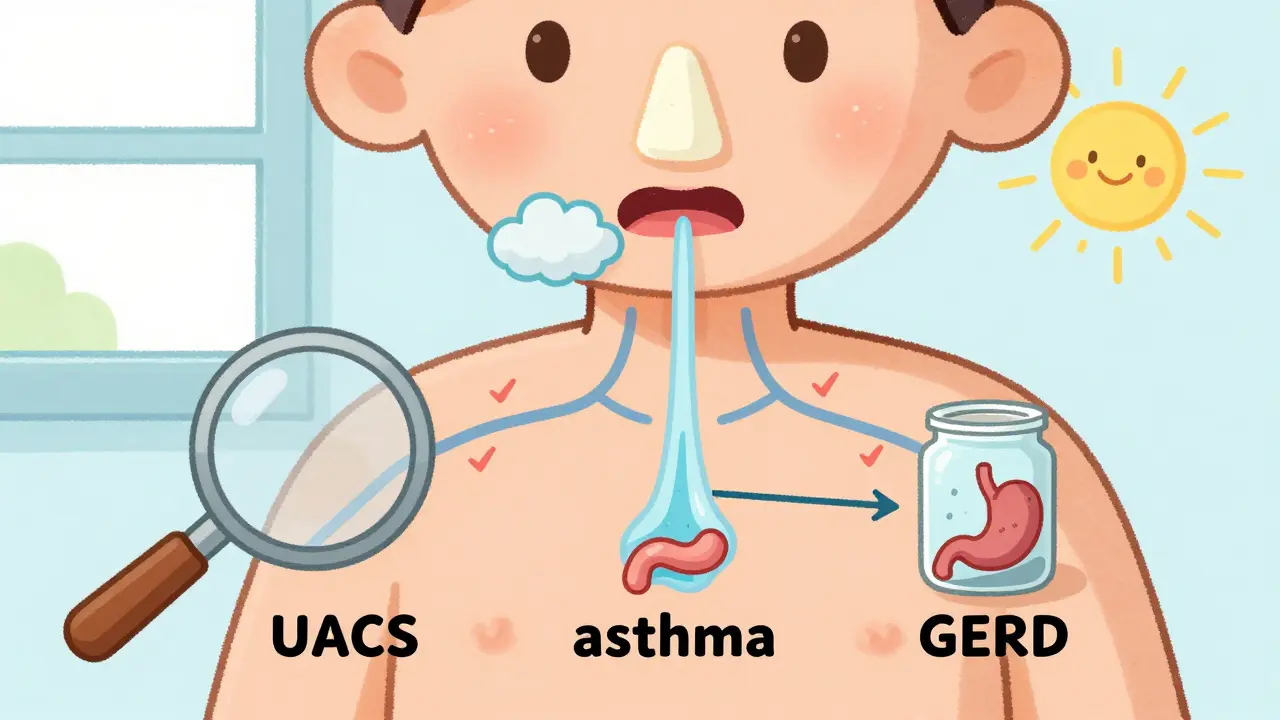
If you’ve been coughing for more than eight weeks, you’re not alone. About 1 in 10 adults deal with a chronic cough, and for most, the cause isn’t pneumonia or a lingering cold-it’s one of three things: GERD, asthma, or postnasal drip (now called upper airway cough syndrome). The good news? There’s a clear, step-by-step way to find out which one is triggering your cough-and fix it without endless tests or guesswork.
What Counts as a Chronic Cough?
A cough that lasts longer than 8 weeks is considered chronic. That’s not just a random number. It’s based on decades of research from the American College of Chest Physicians. Most people assume it’s allergies, a cold, or even stress. But if your cough has been going on for months, it’s likely tied to one of three underlying conditions that affect the airways, throat, or stomach lining. These aren’t rare. Together, they explain 80% to 95% of all chronic cough cases in people who don’t smoke and aren’t taking ACE inhibitor blood pressure meds.
Step 1: Rule Out the Dangerous Stuff First
Before you start testing for GERD or asthma, you need to make sure nothing serious is going on. That means checking for red flags: coughing up blood, unexplained weight loss, night sweats, fever, or a history of lung disease. If any of these are present, you need a chest CT scan or specialist referral right away.
Also, review your medications. ACE inhibitors-like lisinopril or enalapril-cause cough in 5% to 35% of people who take them. The cough usually starts within a week to six months after beginning the drug. If you’re on one of these, switching to a different blood pressure med can resolve the cough in days.
Step 2: The Basic Tests Everyone Needs
You don’t need a fancy scan to start. The first step is simple: a chest X-ray and spirometry.
- Chest X-ray: This rules out tumors, tuberculosis, or bronchiectasis. If it’s normal-which it is in most cases-you can move on.
- Spirometry: This breathing test measures how much air you can force out in one second (FEV1). If your numbers are low, it suggests asthma or COPD. If they’re normal, you might still have cough-variant asthma, which doesn’t show up on spirometry.
These two tests take less than 15 minutes and cost next to nothing. Skip the CT scan unless the X-ray shows something odd. A chest CT exposes you to the same radiation as 74 chest X-rays-and only finds cancer in 1 out of 1,000 people with a normal X-ray.
Step 3: Test for the Big Three-One at a Time
Now you get to the heart of the workup. Doctors don’t test all three at once. They try one, wait, then move to the next. Why? Because each has a clear treatment trial that works if the diagnosis is right.
1. Upper Airway Cough Syndrome (Postnasal Drip)
This is the most common cause, responsible for 38% to 62% of cases. It’s not just mucus dripping down your throat-it’s a hypersensitive cough reflex triggered by irritation in the upper airway. You might notice it more after lying down, in cold air, or around allergens.
The test? A 2- to 3-week trial of a first-generation antihistamine (like chlorpheniramine) plus a decongestant (like pseudoephedrine). You take it twice daily. If your cough improves by 70% or more, it’s UACS. Response usually happens within 7 to 14 days. If no change? Move on.
2. Asthma (Especially Cough-Variant Asthma)
Asthma causes 24% to 29% of chronic cough cases. In cough-variant asthma, the only symptom is coughing-no wheezing, no shortness of breath. It often worsens at night, after exercise, or around cold air.
The test? A 4-week trial of an inhaled corticosteroid (like fluticasone) or a leukotriene blocker (like montelukast). If you’re not sure, a methacholine challenge test can confirm it. A positive result means your airways are overly reactive. Improvement usually shows up in 2 to 4 weeks.
Important: Spirometry can be normal even if you have this. That’s why the treatment trial matters more than the test.
3. GERD (Gastroesophageal Reflux Disease)
GERD causes 21% to 41% of chronic coughs. But here’s the twist: 60% to 70% of people with GERD-related cough don’t have heartburn. It’s silent reflux-stomach acid irritating the throat and voice box without the classic burning sensation.
The test? A 4- to 8-week trial of a high-dose proton pump inhibitor (PPI) like omeprazole 40 mg twice daily. But here’s the catch: only 50% to 75% of people respond. And placebo pills work in up to 40% of cases. That’s why experts now say: don’t just start a PPI without checking for other causes first.
For better accuracy, some clinics use the Hull Airway Reflux Questionnaire (HARQ). A score above 13 suggests laryngopharyngeal reflux with 80% accuracy. It’s free, quick, and available online.
Why This Order Matters
Doctors don’t test these in random order. They go UACS first, then asthma, then GERD. Why?
- UACS responds fastest-within days.
- Asthma trials have high success rates (60-80%).
- GERD trials take the longest and have the lowest success rate.
If you start with GERD and it doesn’t work, you’ve wasted two months and still haven’t ruled out the other two. By testing in order, you cut down on time, cost, and unnecessary meds.

What If None of the Trials Work?
About 10% to 30% of people don’t improve after trying all three. That doesn’t mean it’s “in your head.” It means you might have something rarer:
- Chronic refractory cough (CRC): A condition where the cough reflex is overly sensitive, with no clear trigger.
- Pertussis (whooping cough): Rare in adults, but possible. Requires a nasal swab with special culture.
- Chronic aspiration: Inhaling food or saliva into the lungs, often from swallowing problems.
- Medication side effects: Other drugs besides ACE inhibitors can cause cough.
For CRC, new drugs like gefapixant (approved in 2022) and camlipixant (under FDA review) target the cough reflex directly. They reduce cough frequency by 18% to 25% in clinical trials. These aren’t first-line, but they’re changing the game for people who’ve tried everything.
What Doesn’t Work
Stop wasting time on these:
- Antibiotics: Only 1% to 5% of chronic coughs are bacterial. Most are viral or non-infectious.
- Over-the-counter cough syrups: They rarely help chronic cough. Dextromethorphan works better for acute coughs, not chronic ones.
- Immediate CT scans: Unless the X-ray is abnormal, the risk of radiation outweighs the benefit.
- Empirical PPIs without testing: The FDA and American College of Gastroenterology now warn against this. You’re more likely to get side effects (like bone loss or gut infections) than relief.
What You Can Do Right Now
If you’ve been coughing for months:
- Write down when the cough happens: at night? After meals? In cold air?
- Check your meds: Are you on lisinopril, enalapril, or ramipril?
- Take the HARQ questionnaire (search for “Hull Airway Reflux Questionnaire”).
- Ask your doctor for a chest X-ray and spirometry.
- Don’t start a PPI until you’ve tried the other two causes.
Most people see improvement within 2 to 4 weeks of the right treatment. You don’t need to live with a cough that’s wrecking your sleep, work, or social life. There’s a method. It’s proven. And it works.
Can postnasal drip cause a cough without a runny nose?
Yes. Upper airway cough syndrome (UACS) often causes cough without noticeable nasal drainage. The irritation comes from inflammation in the throat or larynx, not just mucus. People may feel a tickle or need to clear their throat, but not necessarily have a runny nose.
Is a chest X-ray necessary if I have no other symptoms?
Yes. Even if you feel fine, a normal chest X-ray is the first step to rule out serious conditions like lung cancer, tuberculosis, or bronchiectasis. Most chronic coughs are benign, but skipping this test could delay diagnosis of something dangerous.
Why do some people with GERD not have heartburn?
Stomach acid can reach the throat and voice box without triggering the burning sensation in the chest. This is called silent reflux. The throat is more sensitive to acid than the esophagus, so it triggers coughing even when heartburn is absent. Up to 70% of GERD-related cough patients report no heartburn.
Can asthma cause coughing only at night?
Yes. Nighttime coughing is a classic sign of cough-variant asthma. Lying down can trigger airway narrowing, and allergens like dust mites in bedding can worsen symptoms. If your cough gets worse at night and improves during the day, asthma is a strong possibility.
How long should I try a treatment before deciding it’s not working?
For UACS (antihistamines + decongestant): 2 to 3 weeks. For asthma (inhaled steroids): 4 weeks. For GERD (PPIs): 4 to 8 weeks. Don’t stop too early. Improvement can be slow, and placebo effects can make you think it’s working when it’s not. Track your cough frequency daily-use a journal or app-to be sure.
Are new cough medications like gefapixant available now?
Yes. Gefapixant was approved by the FDA in December 2022 for adults with chronic refractory cough. It reduces cough frequency by 18% to 22% compared to placebo. It’s not a first-line treatment-it’s for people who’ve tried all other options and still cough. It’s available by prescription, but insurance coverage varies.

