Neuropathic pain isn't just soreness or a bad ache. It's the kind of pain that feels like electric shocks, burning, or pins and needles-often without any obvious injury. This pain comes from damaged nerves, not from cuts, sprains, or inflammation. About 1 in 10 people live with it. Diabetes, shingles, spinal injuries, and even vitamin B12 deficiency can trigger it. And when it hits, everyday things like a light blanket or a breeze can feel unbearable. That's called allodynia. Or the pain might be way worse than it should be-that's hyperalgesia.
Why Gabapentin and Pregabalin Are First-Line Treatments
For decades, doctors turned to opioids for nerve pain. But they didn’t work well, and the risks were too high. Then came gabapentin and pregabalin. Both were originally made to treat seizures, but in the early 2000s, researchers noticed they calmed down overactive nerves. Now, they’re the go-to medications for neuropathic pain in the U.S. and Europe. The Neuropathic Pain Special Interest Group (NeuPSIG) lists both as first-line options. About 60% of people with nerve pain start with one of these two.
They work the same way: by attaching to a specific part of nerve cells called the alpha-2-delta subunit. This reduces the release of pain signals in the brain and spinal cord. But that’s where the similarities end.
Gabapentin: The Original, But Complicated
Gabapentin (brand name Neurontin) came first-approved for epilepsy in 1993, then for postherpetic neuralgia in 2002. It’s cheap. Generic gabapentin costs about $15 for a 90-day supply of 300mg capsules. That’s why it’s still the top choice in safety-net clinics and rural areas.
But here’s the catch: gabapentin doesn’t behave predictably. Your body doesn’t absorb it evenly. If you take 300mg, you might get 30% absorbed. Take 1,200mg, and absorption drops to 20%. That’s why dosing is tricky. You start low-maybe 100mg at bedtime-and slowly increase every few days. Most people need 3,600mg a day split into three doses. That means remembering to take pills three times a day. Many patients miss doses. One 2023 study found 34.7% of people stopped gabapentin because the dosing was too hard to manage.
Side effects are common: dizziness (26% of users), sleepiness (19%), swelling in the legs (10%), and unsteady walking. Some people say it makes them feel “drugged.” But it rarely causes weight gain-only about 3% of users gain more than 5 pounds.
Pregabalin: Faster, Stronger, But Costlier
Pregabalin (Lyrica) came along in 2004. It’s essentially gabapentin’s upgraded cousin. It binds six times more tightly to the same nerve target. That means it works better at lower doses. A 300mg dose of pregabalin gives you the same pain relief as 3,600mg of gabapentin.
It’s also simpler. You take it once or twice a day. No need to space doses every 8 hours. Most doctors start at 75mg daily and increase to 150-300mg within a week. The 2023 DIRECT-NEUROPATHY trial showed patients reached their effective dose in 8.2 days with pregabalin-almost half the time it took with gabapentin.
It works faster, too. On Reddit, 68% of pregabalin users reported significant pain relief within 3 days. Compare that to 42% for gabapentin. In clinical trials, pregabalin helped 34.5% of diabetic neuropathy patients cut their pain by half-compared to 30% for gabapentin. That might not sound like a big difference, but in chronic pain, even a few percentage points matter.
But it comes with trade-offs. Weight gain is the biggest complaint. About 12% of users gain 5-15 pounds in the first month. Swelling and drowsiness are also more common than with gabapentin. And while gabapentin is generic and cheap, pregabalin still costs around $28 for 60 capsules of 75mg-even after its patent expired. That’s nearly twice the price of gabapentin.

Real People, Real Choices
Online forums are full of stories that mirror the data. One person on Reddit, u/NeuropathyWarrior, said pregabalin dropped their pain from 8/10 to 3/10 in 48 hours-but they gained 12 pounds in six weeks. They switched to gabapentin. It took three weeks to kick in, but no weight gain.
Another user, u/PainFree77, had the opposite experience. Gabapentin made them so dizzy they fell twice in a month. They switched to pregabalin at half the dose and got relief without the dizziness.
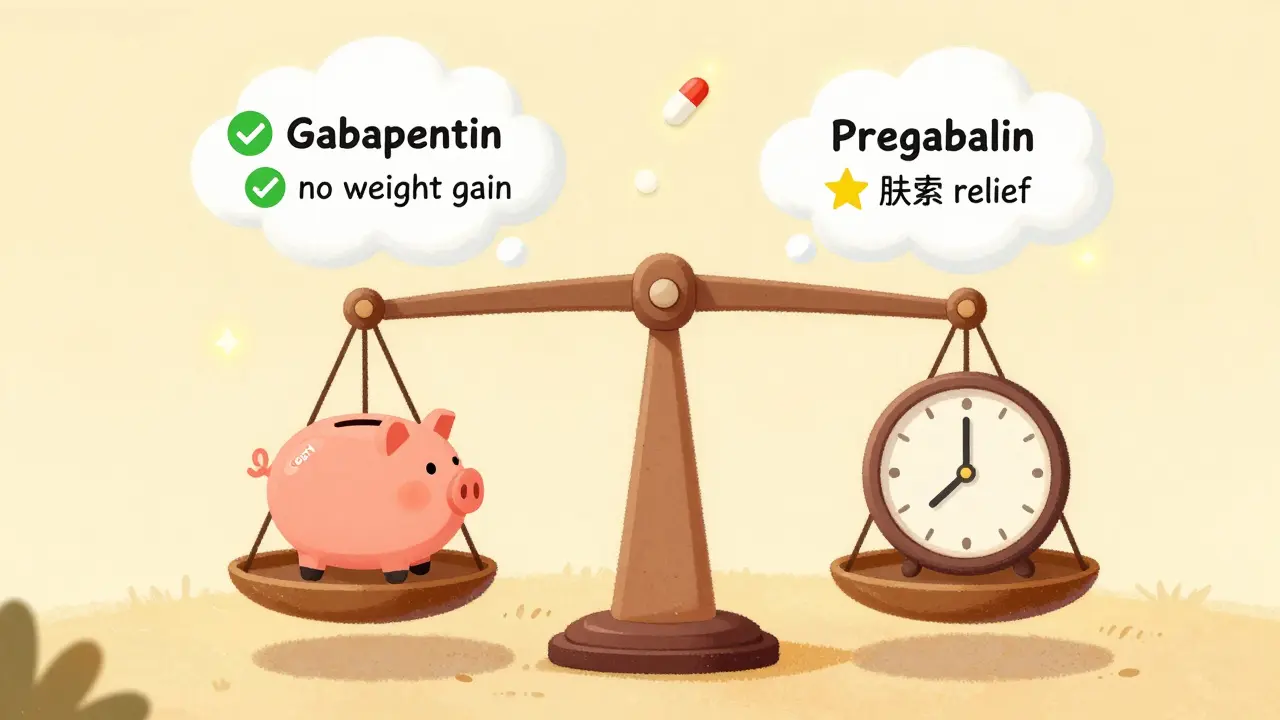
PatientsLikeMe’s analysis of over 3,800 people found pregabalin scored higher for effectiveness (6.2/10) but lower for tolerability (4.8/10). Gabapentin was the reverse: slightly less effective (5.7/10) but better tolerated (5.9/10). So the “best” drug depends on what you value more: speed and strength, or fewer side effects and lower cost.
Who Gets Which Drug?
Doctors don’t just pick one at random. They look at the person.
- If cost is a major issue-especially for Medicare patients or those without insurance-gabapentin wins.
- If someone struggles to remember multiple daily doses, pregabalin’s twice-daily schedule is easier.
- If weight gain is a concern (like for people with diabetes or heart issues), gabapentin is safer.
- If pain is severe and needs fast relief, pregabalin’s quicker onset makes it preferable.
- If the patient has kidney problems, both drugs need dose adjustments, but pregabalin’s predictable absorption makes dosing more reliable.
The American Diabetes Association specifically recommends pregabalin for diabetic nerve pain because of its consistent performance. But the NeuPSIG guidelines say both are first-line-choice depends on individual factors.
The Hidden Risks
Both drugs carry black box warnings from the FDA for suicidal thoughts and mood changes. These are rare-about 0.4% of users-but serious. If someone feels hopeless, withdrawn, or has thoughts of self-harm, they must tell their doctor immediately.
There’s also the risk of withdrawal. Stopping either drug suddenly can trigger seizures, anxiety, or insomnia. You must taper slowly-over weeks, not days. That’s why doctors insist on regular follow-ups.
Pregabalin is now classified as a Schedule V controlled substance in the U.S. because of misuse potential. There were 12.3 overdose deaths linked to pregabalin in 2023, mostly when mixed with opioids or alcohol. Gabapentin has no such classification-and no recorded overdose deaths.
What’s Next?
Newer drugs like duloxetine and venlafaxine (SNRIs) are gaining ground. They’re effective too, with a similar number needed to treat (NNT) of about 6.4. But gabapentin and pregabalin still lead because they’ve been around longer, are well-studied, and have lower addiction risk than opioids.
The extended-release version of pregabalin (Lyrica CR) came out in 2024. It’s once-daily, which improves adherence. Gabapentin enacarbil (Horizant) is also expanding its use beyond nerve pain to restless legs syndrome.
But the big question is whether these drugs will stay first-line. The 2025 NeuPSIG draft guidelines suggest moving them to second-line for some conditions in favor of SNRIs. That’s still being debated. For now, they’re the backbone of nerve pain treatment.
Bottom Line: It’s Not One-Size-Fits-All
There’s no “best” drug between gabapentin and pregabalin. Only the best drug for you.
If you’re on a tight budget, need to avoid weight gain, and don’t mind taking pills three times a day-gabapentin is your friend.
If you need fast relief, hate complex dosing, and can afford the cost-pregabalin might be worth it.
Either way, don’t expect miracles. These drugs reduce pain, not eliminate it. Most people see a 30-50% drop in pain, not total relief. But for many, that’s enough to sleep, walk, or hug their grandkids again.
Work with your doctor. Track your symptoms. Give each drug at least 4-6 weeks to show if it works. And if side effects hit hard, don’t quit cold turkey-talk to your provider. There’s always another option.


Gabapentin’s absorption issues are a nightmare for patients trying to find a stable dose. I’ve seen people bounce between 900mg and 3600mg for months just to get a baseline. The inconsistency isn’t a flaw in the patient-it’s a flaw in the drug design. Pregabalin’s predictable kinetics make it a far more humane option for chronic pain, even if it costs more. Quality of life shouldn’t be rationed by pharmacy tier lists.
Also, the 34.7% discontinuation rate due to dosing complexity? That’s a systemic failure. If a drug requires three-times-daily dosing for efficacy, we need better formulations. Not more patient blame.
I was on gabapentin for 18 months after shingles. I felt like a zombie with a side of wobbly legs. Then I switched to pregabalin-same dose, half the time, and suddenly I could hold my coffee without spilling it. The weight gain? Yeah, I gained 14 pounds. But I could finally hug my daughter without crying. I’d take the extra pounds over the numb, trembling void gabapentin gave me any day.
Also, the FDA black box warning? Real. I had a panic attack after missing a dose. Don’t quit cold turkey. I learned that the hard way.
The pharmacokinetic variance of gabapentin stems from saturable, carrier-mediated absorption via the L-type amino acid transporter 1 (LAT1) in the small intestine-a nonlinear, dose-dependent phenomenon that renders therapeutic drug monitoring nearly useless without plasma assays. Pregabalin, by contrast, exhibits linear pharmacokinetics via passive diffusion, enabling more precise titration and predictable Cmax and AUC profiles.
Additionally, the 2023 DIRECT-NEUROPATHY trial demonstrated a statistically significant reduction in time-to-effective-dose (TTED) with pregabalin (8.2 days vs. 15.9 days; p<0.001), which correlates directly with improved adherence metrics and reduced healthcare utilization in real-world cohorts. The cost differential is irrelevant when factoring in indirect costs of non-adherence: ER visits, lost productivity, caregiver burden.
And yes-weight gain is a class effect mediated by hypothalamic GABAergic modulation of leptin signaling. But it’s manageable with concurrent GLP-1 agonists in metabolic comorbidities. This isn’t a reason to avoid pregabalin-it’s a reason to optimize polypharmacy.
Why do people keep acting like gabapentin is some miracle cheap drug? It’s a joke. Half the people I know on it are just barely functional. And pregabalin? Yeah, it makes you fat. But at least you’re not falling down the stairs. I don’t care if it costs more. My life matters more than a pharmacy’s profit margin.
Also, the fact that gabapentin isn’t even controlled? That’s insane. People are snorting it. And nobody’s doing anything about it. Pregabalin’s Schedule V at least means someone’s paying attention.
As someone who lives in a region where access to specialist care is limited, I find the emphasis on cost and dosing simplicity profoundly important. In rural Canada, where pharmacies are hours away and refrigeration for medications is inconsistent, the predictability of pregabalin’s absorption profile is not merely a pharmacological advantage-it is a lifeline.
Moreover, the cultural stigma attached to chronic pain often leads to delayed diagnosis. When a patient finally receives a prescription, the burden of complex regimens can be overwhelming. The simplicity of twice-daily dosing may be the difference between adherence and abandonment.
Let us not mistake affordability for accessibility. A drug that requires three daily doses may be cheap, but it is not equitable.
USA: Gabapentin is for peasants. Pregabalin is for people who want to live. If you can't afford pregabalin, you're doing something wrong. Get a better job. Get insurance. Stop being a burden on the system. And stop pretending gabapentin is 'good enough'-it's not. It's the pharmaceutical equivalent of duct tape on a broken leg.
Also, the fact that gabapentin isn't controlled? That's a national disgrace. People are mixing it with opioids and dying. We need to ban it. Like, now. 🚫💊💥
Okay, but let’s talk about the real MVP here: the people who actually manage to stick with these meds. You’re not just taking pills-you’re fighting your own nervous system every single day. One day you feel like a superhero, the next you’re crying because your socks feel like sandpaper.
I switched from gabapentin to pregabalin and went from ‘I can’t stand up’ to ‘I can walk to the mailbox without crying.’ Yes, I gained weight. Yes, I’m tired. But I’m alive. And I get to see my dog wag his tail when I come home. That’s worth every extra pound.
Also, if you’re on either of these, you’re a warrior. Don’t let anyone tell you otherwise. 💪❤️
Gabapentin: poor PK, high discontinuation, low efficacy.
Pregabalin: superior binding, faster onset, predictable dosing.
Cost differential irrelevant for chronic conditions.
Weight gain: manageable with lifestyle.
Black box warning: real but rare.
Conclusion: pregabalin > gabapentin in 90% of cases.
Just wanted to say thanks for writing this. I’ve been on pregabalin for three years now. The weight gain was rough, but I finally slept through the night for the first time in a decade. My GP didn’t explain the tapering properly-I nearly had a seizure when I skipped a dose. Please, if you’re reading this: don’t stop cold turkey. Talk to someone. You’re not alone.
And yes, I still buy the generic. Even at $28, it’s cheaper than my last ER visit.